Researchers at CU Anschutz Offer New Insights into HSV-1’s Long-Term Effects
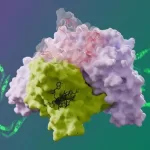
Researchers at the University of Colorado Anschutz Medical Campus have uncovered new details about how the herpes simplex virus type 1 (HSV-1), the virus responsible for the common cold sore, can invade the brain and potentially contribute to neurological diseases like Alzheimer’s. Their study, published today in The Journal of Virology, offers a clearer understanding of how HSV-1 spreads through the central nervous system, highlighting its potential role in neurodegenerative conditions.
Herpes simplex virus type 1 is most commonly known for causing cold sores around the mouth, but recent studies have suggested it might be involved in more serious health conditions, such as Alzheimer’s disease. However, the exact mechanisms behind the virus’s invasion of the brain and its possible link to neurological diseases have remained unclear—until now.
“HSV-1 has been implicated in neurodegenerative diseases, including Alzheimer’s, but no clear route for its invasion into the central nervous system has been established,” said Dr. Christy Niemeyer, an assistant professor of neurology at CU Anschutz and the study’s lead author. “Our study identifies not only how HSV-1 can enter the brain but also which areas of the brain are most vulnerable to infection.”
Mapping HSV-1’s Pathway in the Brain
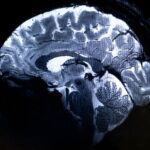
In their groundbreaking study, the research team mapped the virus’s pathway once it enters the brain. They found that HSV-1 doesn’t infect the brain randomly; rather, it targets specific regions crucial to basic functions like sleep, movement, and mood regulation. Notably, the virus was found in the brain stem, which controls essential functions, as well as areas responsible for producing important neurotransmitters such as serotonin and norepinephrine. The hypothalamus, a key region that regulates appetite, sleep, mood, and hormonal balance, was also among the areas affected by the virus.
While HSV-1 did not cause full-blown encephalitis (brain inflammation), its presence still disrupted the function of these vital brain areas. “Even though the virus doesn’t cause overt inflammation, its impact on these regions can affect critical brain functions, which may contribute to long-term neurological damage,” Niemeyer explained.
Microglia and the Long-Term Impact of HSV-1
A particularly significant finding from the study involves microglia, the brain’s resident immune cells. When HSV-1 infects the brain, microglia become inflamed, but in some brain regions, this inflammation persists even after the virus has cleared. The study reveals that this persistent inflammation could play a crucial role in the development of neurological diseases.
“Microglia are the brain’s first line of defense, but when they become chronically inflamed, they can trigger a cascade of immune responses that may lead to neurodegenerative conditions,” said Niemeyer. “Understanding the role of microglia in HSV-1 infection is vital for deciphering how viral infections could contribute to diseases like Alzheimer’s.”
Persistent inflammation in the brain is a well-known factor in the onset of a variety of neurological and neurodegenerative disorders, and this research provides new insights into how viruses, such as HSV-1, may initiate or exacerbate these conditions over time.
Implications for Brain Health
The findings from this study offer important implications for both understanding the broader impact of HSV-1 on brain health and the potential for the virus to trigger widespread neurological diseases. Dr. Niemeyer and her team hope that their research will guide future efforts to develop targeted treatments for HSV-1-related brain infections and potentially prevent the onset of conditions like Alzheimer’s.
“Identifying how HSV-1 invades the brain and understanding the role of microglia in this process are crucial steps toward developing strategies to mitigate the long-term effects of viral infections on brain health,” Niemeyer concluded.
This research is among the first to explore the relationship between HSV-1 and Alzheimer’s disease at this level of detail, and it opens new avenues for exploring how common viral infections may contribute to widespread neurological damage.
Reference: “Olfactory and Trigeminal Routes of HSV-1 CNS Infection with Regional Microglial Heterogeneity” by Christy S. Niemeyer et al., published October 30, 2024, in The Journal of Virology. DOI: 10.1128/jvi.00968-24.