As the landmark TEDDY (The Environmental Determinants of Diabetes in the Young) study nears its conclusion in 2025, new knowledge about type 1 diabetes is emerging, promising to advance understanding and potentially prevent this life-altering condition. Over the next few months, research clinics in Sweden, Finland, Germany, and the United States will collect the final samples from participating children, culminating nearly two decades of extensive research into the disease.
With Sweden and Finland holding the highest incidence rates of type 1 diabetes among children globally, the urgency for understanding the disease’s causes is paramount. Currently, over 1.2 million children and adolescents under 20 are living with type 1 diabetes, and the incidence is rising worldwide. Individuals diagnosed with this autoimmune condition require insulin treatment for survival, making research into its prevention critical.
Initiated in 2004, the TEDDY study encompasses nearly 8,700 children from the four participating countries, focusing on identifying the causes behind type 1 diabetes development. This comprehensive research project has led to numerous publications in high-impact journals, reinforcing the theory that a complex interplay of genetic and environmental factors influences the likelihood of developing the disease.
In anticipation of the final data collection, significant findings from the TEDDY study are detailed in an article published in Nature Reviews Endocrinology. Led by Åke Lernmark, principal investigator in Sweden, the work highlights key insights garnered from the study. Jeffrey Krischer, director of the TEDDY Data Coordinating Center and co-chair of the international study, is a leading co-author.
“The success of this study hinges on the dedication and willingness of the participating children and their families to contribute to our understanding of the disease,” Krischer stated. Many families were motivated by the hope of elucidating the causes of type 1 diabetes and appreciated the close relationships fostered with study coordinators throughout the research process.
Uncovering the Mechanisms Behind Type 1 Diabetes
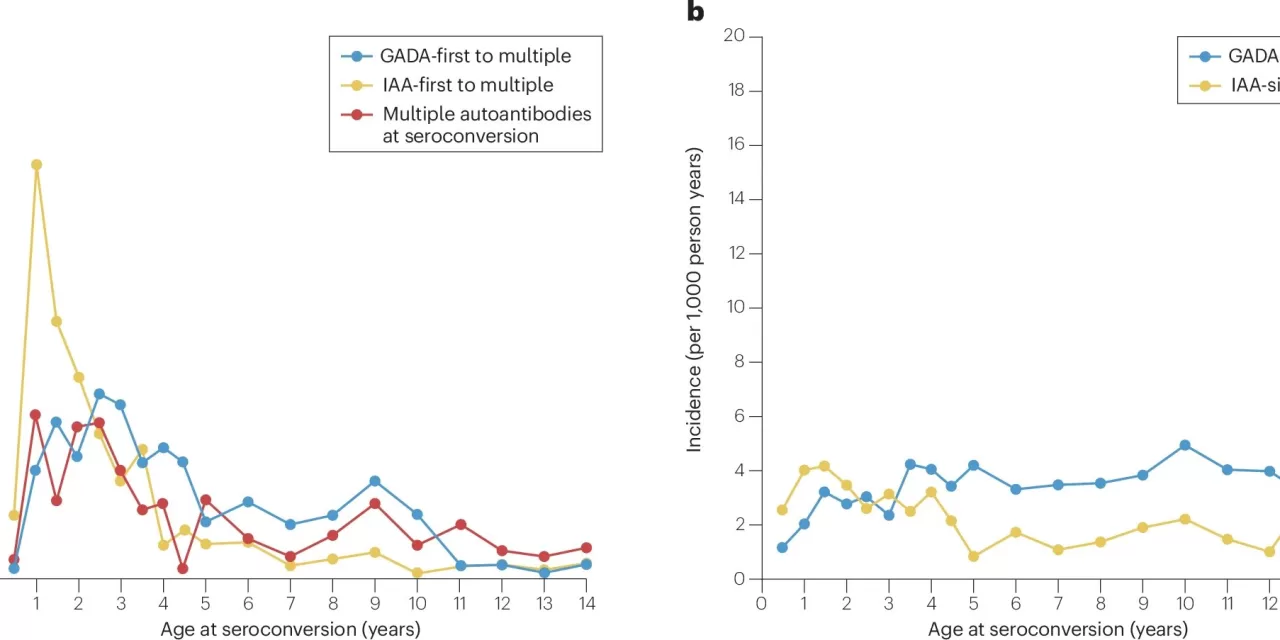
The TEDDY study has meticulously tracked the development of diabetes-related autoantibodies in children, which serve as critical biomarkers for the disease. A blood sample revealing the presence of one of four specific autoantibodies indicates that the pancreas’s insulin-producing cells are being attacked by the body’s immune system. Findings show that autoantibodies against insulin are most prevalent during the first three years of a child’s life, and researchers have identified genetic risk factors that help estimate an individual’s likelihood of developing type 1 diabetes.
Interestingly, the study has revealed that a diagnosis may not occur immediately after the formation of the first autoantibody against insulin, challenging previous assumptions. “We initially thought the disease would be diagnosed shortly after the first autoantibody appeared, but our findings suggest that several years can elapse before a child develops the disease,” Lernmark noted. This insight has amplified interest in systematic screening for type 1 diabetes across various healthcare systems, with genetic risk scores emerging as a vital tool for identifying children who may benefit most from early screening.
Continued Research and Future Directions
The TEDDY study has also illuminated links between enterovirus infections, diabetes-related autoantibodies, and type 1 diabetes. Remarkably, recent findings indicate that administering probiotics to infants at heightened risk may reduce the likelihood of developing diabetes-related autoantibodies.
Research stemming from the TEDDY study continues to thrive, with several new projects currently underway at Lund University Diabetes Center. The POInT study suggests that young children with genetic susceptibility to type 1 diabetes may be at an elevated risk of developing diabetes-related autoantibodies following COVID-19 infection. Similarly, the AVAnT1A study is exploring whether COVID-19 vaccinations can play a preventative role, while the SINT1A study is investigating the potential of probiotics to prevent type 1 diabetes in at-risk children.
Moreover, the TEDDY study has enriched our understanding of other autoimmune diseases, such as celiac disease and thyroiditis. This knowledge feeds into the TRIAD study, which screens children in southern Sweden for type 1 diabetes, celiac disease, and thyroiditis, aiming to develop effective screening methodologies for autoimmune diseases within healthcare systems.
As the TEDDY study approaches its conclusion, researchers remain focused on pivotal questions, particularly regarding the role of viral infections in the development of type 1 diabetes. “If we can clarify the impact of viral infections, we could unlock new avenues for preventing this disease,” Lernmark emphasized.
The findings and insights from the TEDDY study not only pave the way for advancements in diabetes research but also hold the promise of enhancing the quality of life for future generations at risk of type 1 diabetes.
For more detailed insights, refer to the article by Åke Lernmark et al., “Looking back at the TEDDY study: lessons and future directions,” published in Nature Reviews Endocrinology (2024). DOI: 10.1038/s41574-024-01045-0.