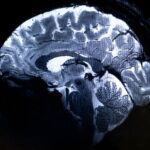
For the first time, researchers have successfully used blood tests to identify concussions caused by intimate partner violence (IPV), a breakthrough that could significantly improve the detection and treatment of brain injuries in IPV survivors. The Monash University-led study, in collaboration with Alfred Health, was published in the journal Brain, Behaviour, and Immunity, and sheds light on a previously hidden aspect of IPV—traumatic brain injuries (TBIs) that often go undetected and untreated.
The study examined symptoms and blood biomarkers in patients who had experienced a concussion within the past 72 hours due to IPV. Among the findings, patients who had suffered a concussion showed worse symptoms and elevated levels of a specific blood biomarker compared to patients without concussion or those whose concussion was caused by other factors.
The study included 10 IPV patients, 80% of whom were women. Notably, 40% had experienced both non-fatal strangulation and concussion. This combination was found to exacerbate the brain injury, highlighting the importance of early detection and intervention in such cases.
Alarming Statistics and Health Implications
Intimate partner violence is a major public health crisis, with one in four Australian women having experienced IPV. It is the leading cause of preventable death, disability, and illness in women aged 15 to 44. Head and neck injuries are the most common in IPV assaults, and nearly 72% of hospital admissions for IPV-related injuries involve these regions, with 12% of admissions due to brain injuries.
Professor Sandy Shultz, a senior author from the Monash University School of Translational Medicine, emphasized that head and neck injuries are among the most significant health challenges for IPV survivors. “Brain injuries caused by IPV are often severe, but detection is difficult because many survivors are reluctant to disclose the type or extent of their injuries,” said Shultz. Consent would be required for the blood test if introduced, which would become part of the overall support system for IPV survivors.
Detecting Concussion in IPV: Unique Challenges
Unlike concussions in sports, concussions caused by IPV are frequently accompanied by strangulation and are often repetitive. This combination can worsen brain injury and lead to severe outcomes if left undiagnosed. One of the main challenges in identifying IPV-related brain injuries is the reliance on self-reporting, which can be unreliable due to fear, memory loss, or the lack of witnesses other than the perpetrator.
“Early identification of brain injuries in IPV patients is crucial to prevent severe consequences, including death,” said Professor Shultz.
Expanding Research for Better Care
The research team is aiming to expand this study into a national, multidisciplinary research program across Australia. The goal is to develop new brain injury detection methods, trial innovative treatments to improve recovery, and implement education programs to enhance health outcomes for this underserved population.
Dr. Georgia Symons, co-first author and a researcher at the Monash Department of Neuroscience, noted that while sports-related concussions have received widespread attention, IPV-related concussions are just as common, if not more so. “The repetitive and combined nature of these injuries in IPV survivors can make them far more dangerous,” said Symons. “There are no mandatory stand-down periods in IPV, which makes recovery more difficult.”
Innovative Animal Models Reveal the Severity of Combined Injuries
To better understand the effects of non-fatal strangulation and concussion, the researchers developed an animal model. This allowed them to study the impact of these injuries both separately and in combination. The results revealed that animals subjected to both strangulation and concussion had more severe cognitive and motor deficits, increased brain inflammation, and higher levels of blood markers indicating brain injury compared to those that experienced only one type of trauma.
Dr. Mujun Sun, another co-first author, explained, “Our findings suggest that blood biomarkers may be a valuable tool for detecting brain injuries in IPV patients, especially when strangulation is involved.”
Looking Ahead
This pioneering research opens the door to better clinical care and management for IPV survivors, potentially saving lives by identifying brain injuries that would otherwise remain hidden. The findings also provide a strong foundation for future research and innovations in detecting and treating brain injuries in this vulnerable population.
The study is a crucial step forward in addressing the silent epidemic of brain injury in IPV and underscores the need for continued research and clinical attention in this area.
For more information, refer to the study: Mujun Sun et al, “Pathophysiology, blood biomarkers, and functional deficits after intimate partner violence-related brain injury,” Brain, Behavior, and Immunity (2024).