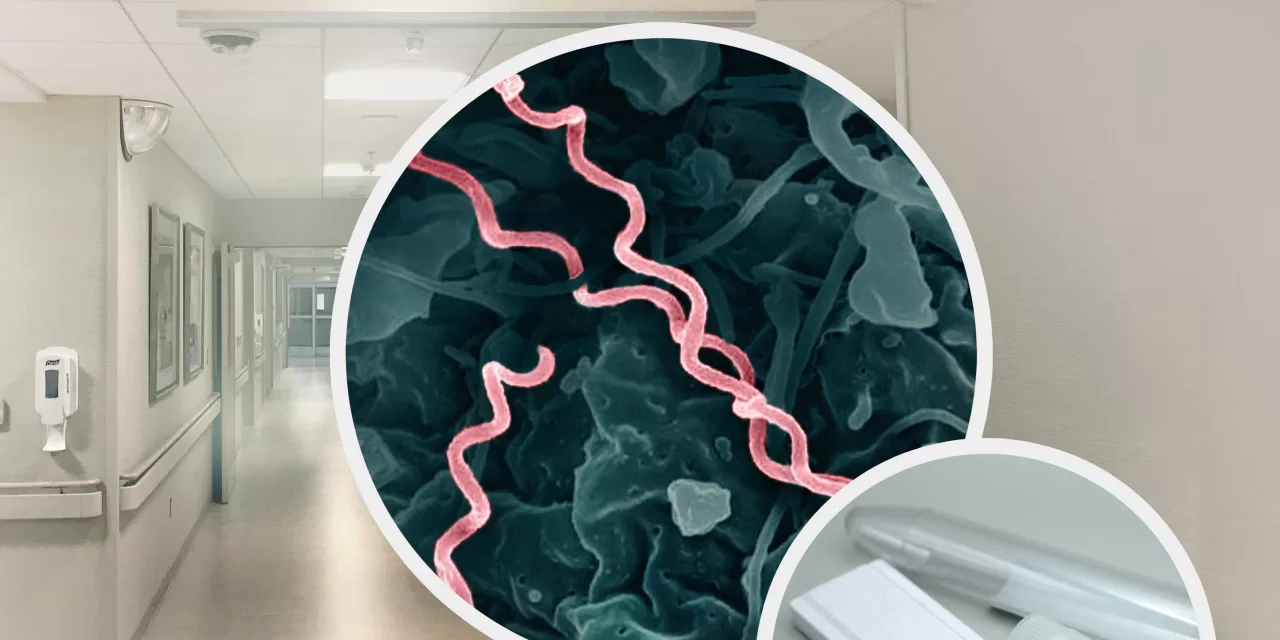
A groundbreaking study supported by the National Institutes of Health (NIH) has unveiled a hidden syphilis epidemic, underscoring the need for expanded testing to combat the rise in cases. The study, published in Open Forum Infectious Diseases, demonstrates that offering optional syphilis tests to individuals seeking care in a large emergency department in Chicago led to a significant increase in screenings and diagnoses—particularly among asymptomatic individuals who would otherwise have gone undiagnosed.
Dramatic Increase in Screening and Diagnosis
The NIH-supported study examined nearly 300,000 emergency department encounters over a four-year period (2017-2021). Researchers implemented an optional syphilis screening strategy for patients aged 18-64, excluding those with documented HIV diagnoses or those recently screened for HIV. The results were striking: testing rates jumped from just 3.6% of patients pre-intervention to 24.4% post-intervention. Diagnoses of presumed active syphilis also rose dramatically, from 161 cases before the intervention to 624 cases afterward.
Most notably, the majority of people diagnosed with syphilis showed no symptoms, revealing that symptom-based screening strategies alone may miss a substantial portion of infections. This highlights the importance of proactive testing approaches in detecting and treating syphilis.
Syphilis on the Rise: A Growing Public Health Concern
The Centers for Disease Control and Prevention (CDC) estimates that syphilis rates have surged in recent years, with adult cases increasing by 80% and congenital syphilis by an alarming 183% between 2018 and 2022. Congenital syphilis, passed from mother to child during pregnancy, can lead to severe complications, including stillbirth and neonatal death.
To tackle this rising epidemic, more effective screening strategies are crucial, especially in populations at risk of undiagnosed infections. These include pregnant women and individuals with limited access to routine healthcare.
Impact on Pregnant People and Congenital Syphilis
The study’s optional testing strategy proved particularly effective in increasing syphilis screenings among pregnant individuals, a critical group for preventing congenital syphilis. Pre-intervention, only 5.9% of pregnant patients received syphilis tests, while post-intervention, nearly half (49.9%) were tested. Confirmed syphilis diagnoses among pregnant people increased from two to 15 cases during the study period, revealing a significant number of missed diagnoses under the prior testing strategy.
The number of concurrent syphilis and HIV diagnoses also rose from seven to 24 without any additional HIV testing intervention, suggesting that expanded syphilis screening may also play a role in identifying co-infections.
A Model for the Future of STI Screening?
The study’s success points to a potential shift in how healthcare providers approach sexually transmitted infection (STI) screening. By offering syphilis testing as part of routine emergency department care, particularly in high-incidence urban areas, healthcare providers can close gaps in diagnosis and treatment for vulnerable populations.
“This approach may help address key healthcare gaps, particularly among pregnant individuals, high-incidence populations, and those with limited access to regular healthcare,” the authors suggest.
As syphilis rates continue to climb, especially among those who may not present with symptoms, the study underscores the importance of integrating proactive screening strategies into broader healthcare settings. This approach could be a critical step in reducing both the personal and public health burdens of untreated syphilis.
Reference
Stanford, K. A., Mason, J., Friedman, E., Hazra, A., Augustine, E., & Schneider, J. (2024). “An Opt-out Emergency Department Screening Intervention Leads to Major Increases in Diagnosis of Syphilis.” Open Forum Infectious Diseases. DOI: 10.1093/ofid/ofae490.
This research was funded by the NIH’s National Institute of Allergy and Infectious Diseases (NIAID).