In 2022, nearly 49,000 people in the United States died by suicide, reflecting a staggering 37% increase in suicide rates since 2000. With suicide now occurring approximately once every 11 minutes, public health officials are increasingly debating the need for universal suicide screening in medical and mental health settings. The practice involves screening all patients for suicide risk, regardless of their reason for visiting. However, this proposed strategy has divided the psychiatric community.
A Growing Call for Universal Screening
The origins of universal suicide screening trace back to a 1999 report by then-U.S. Surgeon General David Satcher, MD. In 2016, the Joint Commission issued an alert recommending healthcare providers improve the detection and treatment of suicidal ideation across all care settings. Data showed that nearly half of those who died by suicide had seen a healthcare professional in the month before their death, yet their risk of suicide was undetected.
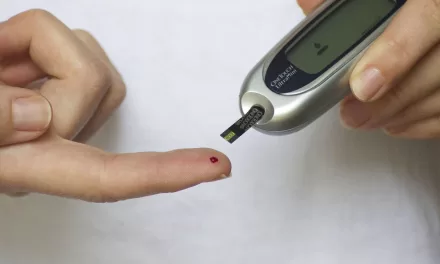
Parkland Health and Hospital System in Dallas was the first U.S. hospital to implement universal suicide screening in 2015. Since then, it has screened more than 4.3 million patients across its emergency department, inpatient units, and primary care clinics. “We’ve been screening between 40,000 to 50,000 patients monthly,” said Kimberly Roaten, PhD, associate chief quality and safety officer for behavioral health at Parkland Health. Clinicians use a five-item tool, the Ask Suicide-Screening Questions, which takes only 20 seconds to complete.
Many other healthcare systems, including the Indian Health Service and the U.S. Veterans Health Administration, have adopted similar universal screening protocols. In California, all acute care hospitals will be required to screen patients aged 12 and older starting in 2025.
Supporters vs. Skeptics
Proponents of universal screening argue it could help identify at-risk individuals who might otherwise go unnoticed, allowing for earlier interventions and potentially saving lives. They point to successful outcomes at facilities like Parkland, where a clinical decision support system integrated into electronic health records classifies patients as low, moderate, or high risk based on their responses to the screening questions.
However, not everyone agrees that universal screening is a silver bullet. Critics, including some mental health professionals, warn about the potential for false positives, especially since suicidal ideation is dynamic and can change rapidly. “Suicidal thoughts can shift within hours,” noted Craig Bryan, PsyD, professor of psychiatry at Ohio State University. He emphasized that even patients who screen positive for suicidal thoughts may not have any intention of acting on them, which could place unnecessary strain on mental health resources.
Dr. Paul Nestadt, associate professor of psychiatry at Johns Hopkins School of Medicine, echoed these concerns. He pointed to research showing that two-thirds of individuals who died by suicide denied experiencing suicidal thoughts shortly before their death. “Suicidal thoughts are very common, but suicide itself is a rare event,” he said. Nestadt advocates for focusing on public health strategies to reduce suicide rates, much like how seatbelt laws and speed limits have reduced motor vehicle fatalities.
Public Health and Policy Solutions
Beyond screening, experts argue that reducing access to lethal means, such as firearms, could have a more significant impact on lowering suicide rates. Studies show that states with stricter gun safety laws experience fewer suicides. Extreme risk protection orders, or “red flag” laws, which allow law enforcement to temporarily remove firearms from individuals at high risk of harming themselves, have also proven effective.
Machine learning models are emerging as another potential solution, with researchers like Nestadt working to create algorithms that flag high-risk patients in medical records, prompting clinicians to intervene as needed.
Innovative treatment approaches, such as brief cognitive behavioral therapy (BCBT), also show promise. Dr. Bryan and his team have demonstrated that BCBT reduces suicide attempts among active-duty soldiers by 60%, with similar success rates in civilian populations.
Moving Forward
While the debate over universal suicide screening continues, one thing is clear: more investment in mental health resources, suicide prevention therapies, and public health policies is crucial to addressing the rising tide of suicide deaths. “We need to train mental health providers and establish risk programs at scale,” Bryan said. “Until we have those interventions in place, we’re putting the cart before the horse.”
As suicide rates continue to climb, the urgency to find effective, scalable prevention strategies has never been greater. Whether universal screening becomes a widespread practice or not, the focus on saving lives remains paramount.