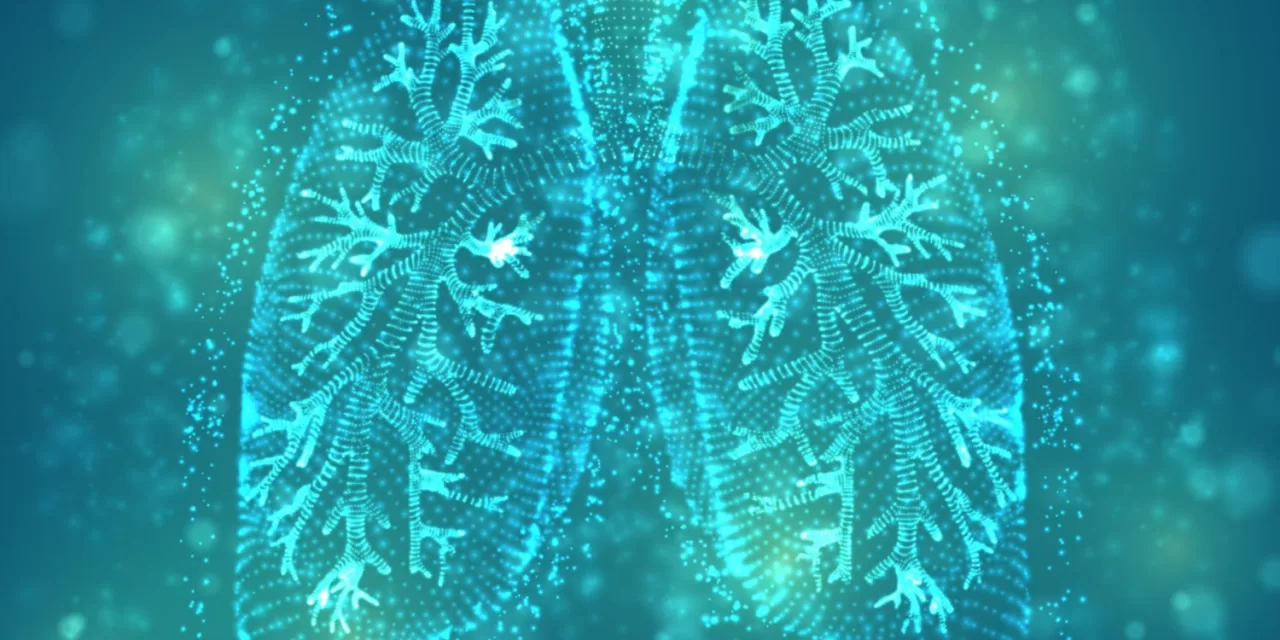
July 27, 2024 — A groundbreaking study suggests that Cordyceps sinensis, a traditional Chinese medicinal fungus, could offer new hope for patients with idiopathic pulmonary fibrosis (IPF), a severe and progressive lung disease. The research, conducted by the Institute of Chinese Materia Medica at the China Academy of Chinese Medical Sciences and published in MedComm-Future Medicine, highlights the potential of Cordyceps sinensis in mitigating the debilitating effects of IPF in a mouse model.
Idiopathic pulmonary fibrosis is characterized by chronic lung inflammation and scarring, leading to a gradual decline in lung function and ultimately respiratory failure. Patients diagnosed with IPF typically face a grim prognosis, with a median survival duration of just 2 to 5 years. Current treatments, primarily antifibrotic medications, often come with significant side effects and do not sufficiently address the disease’s progression.
In this recent study, the researchers investigated the effects of Cordyceps sinensis—a fungus renowned for its antioxidant and anti-inflammatory properties. The findings indicate that this fungus can significantly reduce pulmonary inflammation and collagen deposition in the lungs of mice suffering from IPF.
The study reveals that Cordyceps sinensis appears to exert its therapeutic effects by regulating mitochondrial oxidative phosphorylation. This process helps mitigate the production of mitochondrial reactive oxygen species (mitROS), which are known to contribute to oxidative stress and inflammation. By reducing these harmful factors, Cordyceps sinensis shows promise as a potential treatment for IPF, offering a novel approach to managing this challenging condition.
“Cordyceps sinensis has the potential to be a novel therapeutic agent for IPF, with its effects validated through both in vivo and in vitro experiments,” stated the research team. They emphasized, however, that additional research is necessary to pinpoint the specific components of Cordyceps sinensis responsible for its therapeutic effects and to further elucidate the mechanisms behind its action.
This study marks an exciting development in the search for effective treatments for IPF, potentially paving the way for new therapeutic options that could significantly improve patient outcomes and quality of life.