In a groundbreaking study, researchers at Duke-NUS Medical School have unveiled the initial trigger that sets off severe allergic reactions to substances like peanuts, shellfish, pollen, and dust mites. This discovery, detailed in the April issue of Nature Immunology, opens the door to developing drugs that could prevent these potentially fatal reactions.
Mast cells, a type of immune cell located under the skin, around blood vessels, and in the linings of airways and the gastrointestinal tract, play a central role in allergic responses. When these cells mistakenly identify a harmless substance as a threat, they release a burst of bioactive chemicals. If these chemicals are released simultaneously into the bloodstream, they can cause systemic shock, which can be deadly without rapid treatment.
According to the World Health Organization (WHO), over 10 percent of the global population suffers from food allergies, and the prevalence is rising. Consequently, the incidence of food-triggered anaphylaxis and asthma is also increasing. In Singapore, one in five children has asthma, and food allergies are the primary cause of anaphylactic shock.
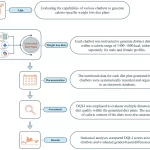
The Duke-NUS research team discovered that the release of bioactive chemicals from mast cells is regulated by two proteins within an intracellular complex called the inflammasome. These proteins, previously known only for their role in secreting soluble chemicals during immune responses, have now been shown to facilitate the movement of particulate mast cell granules to the cell surface, where they are released.
“We discovered that the inflammasome components played a surprisingly crucial role in transporting particulate mast cell granules, which are typically packed in the cell center, to the cell surface where they are released,” said Professor Soman Abraham, Grace Kerby Distinguished Professor of Pathology at Duke University, who led the research. “This surprising discovery gives us a precise target where we can intervene to prevent the cascade of events initiated in mast cells that leads to anaphylactic shock.”
The breakthrough came when the researchers observed that mice lacking either of the two inflammasome proteins, NLRP3 or ASC, did not experience anaphylactic shock when exposed to allergens. However, anaphylactic shock did occur when these proteins assembled and bound to intracellular granules, forming a complex the researchers named granulosome. This complex facilitated the movement of granules along tracks formed by the cytoskeleton within the mast cell.
Dr. Pradeep Bist, co-first author of the paper and a principal research scientist at Duke-NUS, explained: “Upon mast cell activation, we observed rapid granule movement on dynamic tracks known as microtubules to the cell membrane, where these granules were promptly released. However, in mast cells deficient in either NLRP3 or ASC proteins, we found no sign of intracellular granule movement and none of these granules were released.”
The team then tested known inflammasome inhibitors to see if they could prevent this process. Using a drug similar to those in clinical trials for chronic inflammatory diseases, called CY-09, they successfully prevented anaphylactic shock in mice exposed to allergens.
Dr. Andrea Mencarelli, from the Shanghai Jiao Tong University School of Medicine and co-first author, noted: “By employing a drug that specifically blocked inflammasome protein activity, we were able to selectively block the release of mast cells’ pre-stored chemicals without impacting other potentially beneficial activities of mast cells.”
While this is not a cure, it offers a promising new tool for people with severe allergies to prevent traumatic reactions. Current emergency treatments must be administered quickly after the onset of symptoms and can have severe side effects.
“I could see this bringing peace of mind to parents of children with severe food allergies,” said Prof. Abraham. “While we don’t want to deactivate this part of the immune system for prolonged periods, this could potentially provide short-term protection.”
The research team is now focused on optimizing the dosage and frequency of this drug to achieve the best protective effects against anaphylactic shock. They also hope to apply their findings to asthma and allergic skin reactions.
“This breakthrough has tremendous translational potential and represents a paradigm shift not only for further research but more importantly by enhancing the quality of life for those at risk of severe allergic reactions,” said Professor Patrick Tan, Senior Vice-Dean for Research at Duke-NUS. “It’s a beacon of hope, especially for parents of young children who live with this constant concern.”
The study was conducted according to the National Advisory Committee for Laboratory Animal Research (NACLAR) guidelines.