The maxim of resilience and survival is crucial for medically significant fungi. Although these microorganisms are far from recreating the post-apocalyptic scenario depicted in the TV series “The Last of Us,” the lack of attention they have received often leaves them lurking in the shadows. In the bleak landscape of systemic fungal infections, there is a scarcity of precise statistics, clinical histories that include them, simple laboratory tests, new antifungals, and a necessary One Health approach. Here, the only option is to follow the light.
The entomopathogenic fungus Ophiocordyceps unilateralis gained notoriety from the TV series, but for now, it only controls the brains of certain ants. Fortunately, there are no signs that fungi affecting humans are inclined to create zombies.
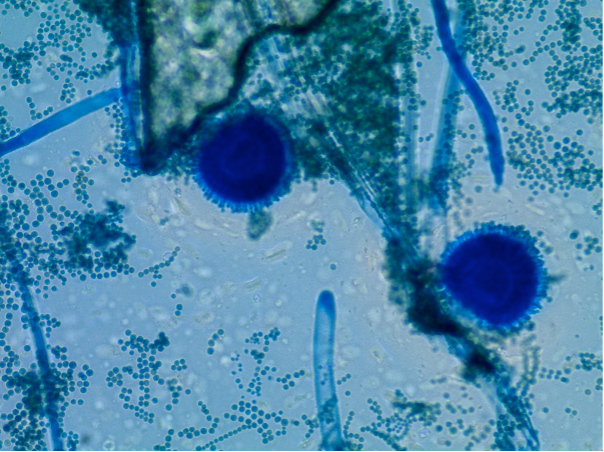
What is clear is that the world belongs to the kingdom of fungi, which are ubiquitous. There are nearly 150,000 described species, with millions yet to be discovered. They thrive in decomposing organic matter, soil, and animal excrement, including that of bats and pigeons. Some fungi have even found a home in hospitals and the human microbiome.
Given such diversity, it’s legitimate to ask whether any fungi could cause new pandemics. Could overlooked species like Cryptococcus neoformans, Aspergillus fumigatus, or Histoplasma trigger health emergencies on the scale of SARS-CoV-2?
We must remember that reality can surpass fiction, as demonstrated by a coronavirus. However, Edith Sánchez Paredes, a biologist and expert in medical mycology, provided a reassuring response: “That would be very difficult to see because fungal infections are not typically acquired from person to person,” she commented from the Mycology Unit of the Faculty of Medicine at the National Autonomous University of Mexico.
Nearly 300 species have been classified as pathogenic in humans, with an estimated 1,500,000 people worldwide dying annually from systemic fungal infections. “The establishment of an infection depends not only on the causal agent but also on the host, in this case, the human,” Sánchez Paredes explained. Generally, these infections develop in individuals with compromised immune systems.
The possibility of a fungal pandemic like SARS-CoV-2 in the short term is remote, but the threat of fungal infections persists. In 2022, the World Health Organization (WHO) defined a priority list of pathogenic fungi to guide control actions, highlighting the rise of invasive fungal diseases, particularly in immunocompromised populations.
“Despite growing concern, fungal infections receive very little attention and resources, leading to a paucity of quality data on fungal disease distribution and antifungal resistance patterns,” the WHO document states. This sentiment is echoed in a 2022 Mycoses article, which concludes that fungal infections are neglected diseases in Latin America.
Access to tests such as polymerase chain reaction or serum detection of beta-1,3-D-glucan is often limited, and treatments like liposomal amphotericin B and new azoles such as posaconazole and isavuconazole are hard to come by in many countries.
“Unfortunately, in Latin America, we suffer from poor infrastructure for diagnosing fungal infections and limited access to antifungals available in the global market,” said Rogelio de Jesús Treviño Rangel, a medical microbiologist and expert in clinical mycology.
Need for More Medical Mycology Training Dr. Fernando Messina, a medical mycologist at the Francisco Javier Muñiz Infectious Diseases Hospital in Buenos Aires, Argentina, has observed an increase in cases of cryptococcosis, histoplasmosis, and aspergillosis. “Particularly, pulmonary aspergillosis is steadily increasing due to structural lung alterations from diseases like tuberculosis and chronic obstructive pulmonary disease,” Messina stated.
For Messina, the main obstacle is the low awareness among nonspecialist physicians regarding systemic fungal infections. “Health professionals usually do not think about mycoses because mycology occupies a very small space in medical education,” he explained. He emphasized the need for more education in mycology at both undergraduate and postgraduate levels.
Messina sees it as unlikely that a fungal pandemic will occur soon, but he believes it would heavily impact regions with inadequate healthcare infrastructure. “We need more doctors, biochemists, and microbiologists trained in mycology,” he stressed.
More than 40 interns, including doctors and biochemists from various regions, pass through Muñiz Hospital each year to enhance their training in mycology. Gabriela Santiso, head of the Mycology Unit at the same hospital, highlighted the importance of rapid diagnostic methods and traditional techniques for identifying fungi and determining resistance to antifungals.
Why Are Resistant Fungal Infections Becoming More Common? Most fungi cannot withstand body temperature or evade the immune response when they try to enter the body. However, if the immune system is compromised, fungi like Candida albicans can lead to serious infections. The WHO attributes the rise in fungal infections to the increased prevalence of immunosuppressive diseases, greater access to critical care units, and invasive medical procedures.
Environmental factors also play a role. “Fungi have enzymes and proteins that help them survive in stressful environments, aiding them in evading the immune system and antifungals,” said Sánchez Paredes. Climate change may also contribute to the rise in fungal infections by enabling fungi to adapt to higher temperatures.
One Health in Fungal Infections The growing resistance to antifungals underscores the interconnectedness of human, animal, and environmental health. A multidisciplinary One Health approach is essential for managing fungal infections. “The use of agricultural fungicides structurally similar to clinical azoles generates resistance in Aspergillus fumigatus found in the environment,” explained Dr. Carlos Arturo Álvarez, an infectious diseases physician.
Álvarez called for better coordination between agriculture, animal and human health sectors, academia, and international organizations to implement the One Health approach effectively.
Veterinary public health is another crucial aspect. Carolina Segundo Zaragoza, who heads the veterinary mycology laboratory at the National Autonomous University of Mexico, has observed frequent consultations for cutaneous mycoses linked to animal contact. She emphasized the need for standardized criteria for detecting, diagnosing, and treating mycoses in both humans and animals.
Alarms Sound for Candida auris The WHO included Candida auris in its group of critical priority pathogens due to its high transmissibility and mortality rate in hospitals. “It shows resistance to most clinically used antifungals and causes epidemic outbreaks,” Sánchez Paredes emphasized. The fungus has been linked to nosocomial infections in critically ill patients, particularly those with prolonged hospital stays and invasive medical devices.
Open Ending As seen in some science fiction series, fungal infections still have an open ending. With better diagnostics and treatments, deaths caused by fungi could decrease significantly. However, if current trends continue, emerging and reemerging fungi resistant to all established treatments may create a chaotic scenario.
“Therapeutic failure due to multidrug resistance could make it catastrophic,” Sánchez Paredes summarized. Currently, there are only four families of drugs capable of counteracting fungal infections, and some are already scarce in Latin America’s hospital pharmacies.
“Fungal infections have historically been given less importance than those caused by viruses or bacteria,” said Treviño Rangel. He pointed out that the main limitation for developing new drugs is economic, as pharmaceutical companies are reluctant to invest in antifungal research without sufficient knowledge of disease incidence and prevalence.
Vaccines to prevent fungal infections face similar barriers, compounded by the similarity between fungal and human cells, which can lead to harmful cross-reactivity. Meanwhile, fungi continue to resist and survive, adapting to new environments over millions of years.
While a fungal pandemic like SARS-CoV-2 seems unlikely in the short term, the threat of emerging and reemerging fungi resistant to established treatments remains a concern for the future.