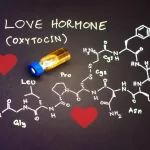
A recent comprehensive review of healthcare systems across high-income countries, including the US, Germany, Canada, and South Korea, has cast doubt on the benefits of healthcare privatisation. Published in The Lancet Public Health journal, the study led by researchers from the University of Oxford challenges the notion that privatisation leads to improved healthcare quality through market competition and flexibility.
Contrary to expectations, the researchers found that transitioning healthcare facilities from public to private ownership often resulted in higher profitability, primarily achieved through cost-cutting measures such as reducing staff and limiting services for patients with insufficient insurance coverage. This pursuit of higher profits was associated with adverse outcomes, including increased rates of avoidable deaths in some instances.
Dr. Aaron Reeves, co-author of the study from the Department of Social Policy and Intervention at the University of Oxford, cautioned against viewing privatisation as a panacea for healthcare challenges. “Outsourcing services to the private sector does not consistently deliver better or more cost-effective care,” Dr. Reeves noted. This finding carries significant implications for policymakers globally, especially in light of ongoing health system strains exacerbated by the COVID-19 pandemic.
The study’s relevance extends beyond high-income countries. Vikash R. Keshri, a health policy and systems researcher, emphasized its applicability to low- and middle-income countries like India. “The experiences of high-income countries underscore the risks of privatisation without robust regulatory frameworks,” Keshri highlighted, noting that weaker regulatory environments could exacerbate disparities in healthcare access and quality.
Keshri, corresponding author on a related study exploring national health policy in India, expressed concerns over the dominance of government entities in health policy decision-making. “Centralisation of health policy processes in India limits diverse perspectives and may hinder effective implementation at regional levels,” Keshri explained. This centralisation trend, he argued, could undermine the responsiveness and inclusivity needed to address varied healthcare needs across India’s diverse population.
Reflecting on the lessons from the COVID-19 pandemic, Keshri stressed the importance of resilient public health systems. “Public health systems, accountable to the people, play a crucial role during crises when market-driven approaches falter,” he asserted. However, he advocated for strengthened regulations to ensure that the private sector contributes effectively and responsibly during emergencies.
As governments worldwide navigate healthcare reform amidst evolving challenges, the study serves as a critical reminder of the complex dynamics and potential pitfalls associated with healthcare privatisation. Balancing private sector involvement with robust regulatory oversight emerges as a pivotal consideration in shaping equitable and effective healthcare systems for the future.