In a groundbreaking study, researchers from the Wyss Institute for Biologically Inspired Engineering at Harvard University, along with collaborators from Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and Genentech, have unveiled a novel approach to boost and prolong lymph node (LN) expansion. This discovery could potentially revolutionize vaccine efficacy, particularly in the context of cancer immunotherapy. Their findings, published in Nature Biomedical Engineering, shed light on how prolonged LN expansion impacts the immune system and the effectiveness of vaccines against tumors.
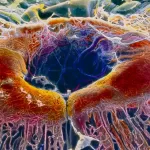
Lymph nodes, crucial hubs in the immune system, play a pivotal role in filtering lymph fluid and orchestrating immune responses. While past research has delved into the initial expansion of LNs following vaccination, little was known about the effects of sustained LN expansion on vaccine outcomes. The team’s innovative method involved a biomaterial vaccine formulation designed to induce greater and more persistent LN expansion compared to conventional vaccines.
Lead researcher David Mooney, Ph.D., emphasized the significance of their approach, stating, “By enhancing the initial and sustained expansion of LNs with biomaterial scaffolds, [we] tightly correlate a persistent LN expansion with more robust immune and vaccination responses.” This breakthrough opens new avenues for immunology research and holds promise for future vaccine development.
The team’s prior work had laid the groundwork for biomaterial scaffolds in cancer and infection vaccines. However, they had yet to explore how these vaccines influence LN responses and their subsequent impact on vaccine efficacy. Through their study, they demonstrated that the biomaterial vaccine formulation, based on microscale mesoporous silica rods, induced profound changes in LN dynamics, tissue organization, and immune cell populations.
Utilizing advanced imaging techniques such as high-frequency ultrasound (HFUS), the researchers tracked individual LNs in vaccinated mice over an extended period. They observed a significant and sustained expansion of LNs, far surpassing those in mice receiving traditional vaccines. Moreover, mechanical analyses revealed alterations in LN stiffness and viscosity, indicative of profound structural changes.
Of particular interest were the shifts in immune cell populations within expanding LNs. The vaccine triggered a cascade of immune responses, mirroring those seen in typical infectious scenarios. Notably, “innate immune cells” surged initially, followed by dendritic cells (DCs) and adaptive immune cells crucial for mounting targeted immune responses against pathogens or tumors.
Collaborating with experts in lymph node biology, the team elucidated the role of myeloid cells in LN expansion and vaccine efficacy. Through single-cell RNA sequencing, they identified specific myeloid cell populations whose gene expression profiles correlated with LN expansion. Manipulating these cell populations affected the maintenance and timing of immune responses, highlighting their significance in vaccine outcomes.
Most significantly, priming LNs with the biomaterial vaccine prior to administering traditional antigens led to enhanced anti-tumor immunity and prolonged survival in melanoma-bearing mice. This strategy holds promise for future vaccine developments, offering a novel means to bolster immune responses against various diseases, including cancer.
Donald Ingber, M.D., Ph.D., Founding Director of the Wyss Institute, underscored the broader implications of the study, emphasizing the pivotal role of mechanics in immune regulation. He expressed optimism about the potential of this approach to bolster immunotherapies and enhance patient outcomes.
The study, funded by the National Institutes of Health/National Cancer Institute, represents a significant advancement in vaccine research, with far-reaching implications for immunotherapy and disease treatment.