A recent study conducted by The University of Texas MD Anderson Cancer Center suggests that altering cessation regimens and increasing medication doses significantly enhances the likelihood of smokers successfully quitting. The study, published in JAMA, compared the effectiveness of varenicline, a cessation medication, with combined nicotine replacement therapy (CNRT), such as patches or lozenges.
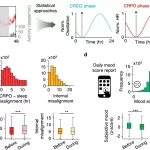
The research, led by Dr. Paul Cinciripini, Chair of Behavioral Science at MD Anderson, followed 490 smokers who were randomly assigned to either varenicline or CNRT for a six-week period. Those who were unable to quit during this phase were then re-randomized to either continue with the same treatment, switch treatments, or increase the dosage for an additional six weeks.
The findings revealed that smokers who initially failed to quit with varenicline were seven times more likely to succeed by the end of the second phase if their varenicline doses were increased. Moreover, there was nearly a two-fold increase in successful quit attempts for those who switched from CNRT to varenicline. Conversely, patients who switched from varenicline to CNRT or remained on the same treatment plan had minimal success in quitting.
Dr. Cinciripini emphasized the importance of flexibility in cessation treatment, stating, “Sticking to the same medication isn’t effective for smokers who are unable to quit in the first six weeks of treatment.” He urged healthcare providers to monitor patients closely and consider alternative approaches, such as increasing medication dosage, for those struggling to quit.
The study, conducted between June 2015 and October 2019 in Texas, highlights the critical role of tailored cessation interventions, particularly given the persistent challenges posed by tobacco addiction. Tobacco use remains the leading preventable cause of death and disease in the U.S., with over 480,000 Americans succumbing to tobacco-related illnesses annually.
Moreover, quitting tobacco can significantly improve survival rates for cancer patients who smoke by 30–40%. Recognizing the importance of addressing barriers to cessation, MD Anderson continues to explore innovative strategies at both individual and population levels, including cost-effective interventions and enhanced access to cessation services.
Looking ahead, MD Anderson researchers are conducting a larger ongoing trial to evaluate various medication combinations as alternatives for individuals who fail to quit on their initial varenicline or CNRT doses. These efforts signify a concerted commitment to combating tobacco addiction and reducing the burden of smoking-related diseases.
Source: [JAMA (2024)](jamanetwork.com/journals/jama/ … .1001/jama.2024.4183)