The World Health Organization today called on countries in WHO South-East Asia Region to prioritize transition from long-stay institutional mental health services to community-based care, to ensure these services are accessible, equitable, and stigma-free, and the affected individuals provided opportunities to lead a productive life.
“Transitioning from long-stay tertiary psychiatric institutions to community-based care is beneficial for both individuals and society at large. When these services are integrated into the fabric of our communities, it becomes easier for individuals to seek help without the fear of judgment or discrimination. This shift also allows for greater personal autonomy, improved quality of life, and personalized care options. The community-based settings provide individuals opportunities to regain a sense of independence and engage in social and vocational activities, which can significantly improve their overall well-being,” said Ms Saima Wazed, Regional Director WHO South-East Asia, in her virtual address to the regional meeting on ‘Transitioning from long-stay services to community mental health networks: towards deinstitutionalization in WHO South-East Asia Region’.
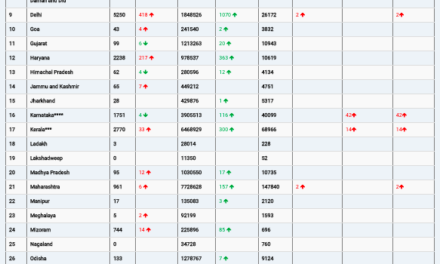
An estimated 13.7% of the populations of the Region suffers from mental health conditions. The treatment gap for mental health conditions remains high – as high as 95%. More than 200 000 people die of suicide every year. People with severe mental disorders die 10 to 20 years earlier than others. However, investment in mental health remains very low across the Region.
The Regional Director released a report on ‘Deinstitutionalization of people with mental health conditions in WHO South-East Asia Region’, which while acknowledging the complexities and unique contexts of each country, offers recommendations that can be adapted to local realities.
“This report can serve as a catalyst for change, igniting a process that results in every person leading a life of dignity, purpose, and fulfilment,” said Ms Wazed, who champions the cause of mental health and has set it as one of her top priorities as Regional Director.
Long-stay mental health institutions, including psychiatric hospitals and asylums, are often characterized by the absence of effective treatment, segregation, poor living conditions, lack of resources, and overcrowding. The transition from institutional care to community-based care is driven by a growing understanding of the negative impact of long-term institutionalization, advances in treatments, and recognition of the human rights and dignity of individuals with mental disorders.
“Historically mental health care has been synonymous with institutionalization. Large asylums were built with the intention of providing a place of refuge for those grappling with mental illnesses. However, as our understanding of mental health has evolved, so too must our methods of care,” the Regional Director said.
Earlier, the Paro Declaration on universal access to people-centered mental health care and services, adopted by Member countries of the Region in 2022, and the Regional Action Plan for Mental Health for the WHO South-East Asia Region 2023-2030, emphasized on the shift to community-based services.
Besides being more efficient, community-based services are also better equipped to identify mental health concerns at an early stage, reducing the need for crisis intervention. This approach benefits individuals, alleviates the burden on emergency services and reduces the overall cost of mental health care, she said.
Importantly, community-based mental health care shows better outcomes, reduces treatment gap, and increases coverage.
Community-based care models emphasize on the creation of safe and supportive living environments within the broader society, which not only benefits individuals with mental disorders but also promotes empathy and understanding among the public, dispelling misconceptions, and reducing stigma.
Successful deinstitutionalization, moving from tertiary care to community care, requires careful planning, collaboration, additional financial resources, and continuous monitoring. It needs parallel expansion of community care services and networks.
Adequate community resources, including housing, employment opportunities, vocational training, empowerment of people with lived experience and caregivers and social support networks must be established to facilitate a smooth transition from institutional care and integration and reintegration into community living.
Comprehensive training programs for mental health professionals, law enforcement, educators, and community members are essential to ensure that individuals with mental disorders are treated with respect and understanding, for their full inclusion and participation into communities.
The process of deinstitutionalizing is a complex undertaking that requires careful consideration of cultural, social, economic and policy factors. The three-day regional meeting being held in Bangkok, Thailand, will deliberate on issues and challenges and the way forward for deinstitutionalization for improved mental health outcomes, enhanced social integration and human rights.