January 14, 2024
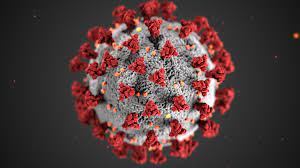
Long COVID, a condition affecting at least 65 million people globally, continues to be a perplexing health challenge, with symptoms persisting for months after the onset of initial COVID-19 symptoms. A recent study by researchers from the Amsterdam University Medical Center, published in the journal Nature Communications, has provided insights into the physical roots of long COVID fatigue, uncovering abnormalities in muscle tissue, particularly mitochondrial dysfunction.
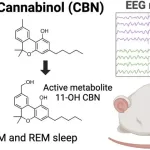
Long COVID is marked by symptoms such as fatigue, dizziness, mobility issues, sleep problems, cognitive impairment, and brain fog. These symptoms can significantly impact individuals’ lives, as revealed by a study highlighting the severe disruption of work, home, social, and private lives for over half of those affected.
The Amsterdam University Medical Center’s study aimed to identify the physical cause of fatigue in long COVID patients, recognizing the profound impact on their daily lives. The research, led by Prof. Michèle van Vugt, involved a cycling test for 25 individuals with long COVID and 21 healthy participants. The test triggered post-exertional malaise, resulting in worsening fatigue for up to 7 days after.
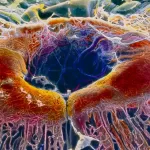
Blood and muscle tissue samples were collected from all participants before and after the cycling test. The study found abnormalities in the muscle tissue of those with long COVID, specifically lowered functioning of the mitochondria—the cell’s powerhouse responsible for generating energy.
Prof. van Vugt emphasized the biological basis of fatigue in long COVID, stating, “The brain needs energy to think. Muscles need energy to move. This discovery means we can now start to research an appropriate treatment for those with long COVID.”
The unexpected findings related to muscle tissue abnormalities have prompted the research team to explore whether similar alterations exist in other post-infectious patients, seeking to uncover the cause of these muscle changes and potential treatment avenues.
Dr. David Cutler, a family medicine physician not involved in the research, noted that this study contributes to reassuring long COVID sufferers that their experiences are physically real, not just psychological. While acknowledging the challenges in treating long COVID, he emphasized the importance of reassurance, thorough evaluation, and the endorsement of the long COVID diagnosis. Dr. Cutler suggested that future research could explore various regimens of exercise, nutritional support, and emotional therapy to alleviate the suffering of those with long COVID.