Description of the Situation
Global Overview
Current situation
The global incidence of dengue has markedly increased over the past two decades, posing a substantial public health challenge. From 2000 to 2019, the World Health Organization (WHO) documented a ten-fold surge in reported cases worldwide increasing from 500 000 to 5.2 million. The year 2019 marked an unprecedented peak, with reported instances spreading across 129 countries.
After a slight decline of cases between the year 2020-2022 due to the COVID-19 pandemic and lower reporting rate, in 2023, an upsurge in dengue cases have been observed globally, characterized by a significant increase in the number, scale, and simultaneous occurrence of multiple outbreaks, spreading into regions previously unaffected by dengue.
Dengue transmission is cyclic and large outbreaks every 3-4 years can be expected. During the COVID-19 pandemic we saw moderate transmission of dengue in some regions and low transmission in others leading to an accumulation of people without immunity to certain dengue virus serotypes. However, the data on the circulating dengue serotypes is limited.
Since the beginning of 2023, ongoing transmission, combined with an unexpected spike in dengue cases have resulted in close to a historic high of over five million cases and more than 5000 dengue-related deaths reported in over 80 countries/territories and five WHO regions: Africa, Americas, South-East Asia, Western Pacific and Eastern Mediterranean Regions globally (Figure 1). Close to 80% of these cases, or 4.1 million, have been reported in the Region of the Americas. Dengue is the most widespread arbovirus and causes the highest number of arboviral disease cases in the Region of the Americas, with cyclic epidemics recurring every 3 to 5 years. In addition, clusters of autochthonous dengue have been reported in the WHO European Region. However, these numbers are likely an underestimate of the true burden as most of the primary infections are asymptomatic and dengue reporting is not mandatory in many countries.
Several factors are associated with the increasing risk of spread of the dengue epidemic including, the changing distribution of the vectors (chiefly Aedes aegypti and Aedes albopictus), especially in previously dengue naïve countries; the consequences of El Nino phenomena in 2023 and climate change leading to increasing temperatures and high rainfall, humidity among others; fragile health systems in the midst of COVID-19 pandemic, political and financial instabilities in countries facing complex humanitarian crises and high population movements. These factors also challenge the response to the epidemic and the risk of further spread to other countries. Weakness in the surveillance systems in many affected countries may have led to delayed reporting and response and missed identification of symptoms, contributing to increased severe dengue outcomes.
WHO has assessed the risk to be high globally considering the increasing risk of transmission and the upsurge of cases and deaths.
Figure 1: Countries/territories/areas reporting autochthonous dengue cases (November 2022- November 2023) *
* Based on most recent available data (the data should be interpreted considering the differences in reporting rates and case definitions between the regions).
Regional overview
WHO Region of Africa:
Africa is among the top four regions most affected by arboviral diseases, including yellow fever, dengue, chikungunya, O’nyong nyong, Rift Valley fever, and Zika. In 2023, 171 991 dengue cases have been reported in countries in the region and 753 deaths. Evidence of dengue circulation has been detected in local populations and/or among travelers returning from more than 30 African countries.
Outbreaks have been reported from 15 of the 47 countries including Benin, Burkina Faso, Cape Verde, Chad, Côte d’Ivoire, Ethiopia, Ghana, Guinea, Mali, Mauritius, Niger, Nigeria, São Tomé and Principe, Senegal and Togo. The outbreaks in most of these countries began in 2023, except in São Tomé and Príncipe, where it was a continuation of an outbreak that started in April 2022. As of 19 December 2023, outbreaks are still ongoing in 11 countries and were declared over in Chad, Guinea, Mauritius, and São Tomé and Príncipe.
The most affected country in the region in 2023 is Burkina Faso, experiencing a significant increase in dengue cases compared with the same periods in 2021 and 2022. As of 18 December, the cumulative number of cases reported in the country for 2023 is 146 878 suspected cases, including 68 346 probable cases (positive rapid diagnostic test) and 688 deaths among suspected cases, representing a case fatality rate of 0.5%.
The burden of dengue in Africa is not well understood due to i) similarity of common, non-specific clinical symptoms of the disease with malaria and other tropical febrile illnesses; ii) limited laboratory capacity for timely detection and confirmation of dengue, which is crucial for detecting and reporting cases and preventing its spread; and iii) inadequate surveillance and limited case reporting, especially for dengue.
Efforts are ongoing to better understand the transmission dynamics of dengue and other arboviruses in the region. The WHO Regional Office for Africa has endorsed the Framework for the integrated control, elimination and eradication of tropical and vector-borne diseases in the African Region 2022-2030. Equally, the Regional Office has also drafted the Framework for implementation of the Global Arbovirus Initiative by targeted Member States in the WHO African Region.
WHO Region of the Americas:
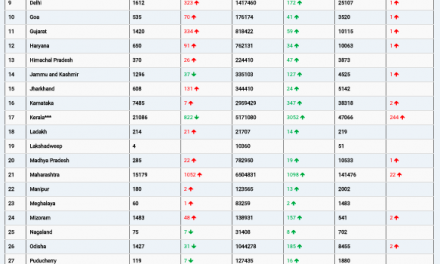
Between 1 January 2023 and 11 December 2023, a total of 4.1 million suspected dengue cases (cumulative incidence of 419 cases per 100 000 population), including 6710 severe cases (0.16% of suspected cases) and 2049 deaths (CFR 0.05%) were reported from 42 countries and territories in the Region of the Americas, with 15 countries reporting active outbreak. Of the total number of dengue cases until 12 November 2023 (EW 48 of 2023), 1 895 122 (45%) were laboratory confirmed.
Currently, 46 countries and territories systematically report, through the Health Information Platform for the Americas (PLISA), on a weekly basis, the total number of cases, incidence, number of severe cases, number of deaths and lethality due to dengue, as well as entomological surveillance data. As of EW 48, Brazil has reported the highest number of suspected cases in the Region (n = 2 909 404; 1359 cases per 100 000 population), followed by Peru (n= 271 279; 813 cases per 100 000 population), and Mexico (n = 235 616; 179 cases per 100 000 population). In terms of severe dengue, Colombia reported the most cases (1504; 1.35% of cases), followed by Brazil (1474; 0.05% of cases), Mexico (1272; 0.54% of cases), Peru (1065; 0.39% of cases), and Bolivia (640; 0.44% of cases).
Although dengue is endemic in most countries of South America, Mexico and Central America, and the Caribbean countries, the second half of 2023 has witnessed an alarming increase in cases, with cumulative cases for the year surpassing all previous yearly totals and in some countries extending beyond historically affected areas of transmission. Dengue cases have increased in the Americas over the past four decades, from 1.5 million cases from 1980 to 1989 to 17.5 million in 2010-2019. Before 2023, the highest historical dengue caseload was in 2019, with over 3.18 million cases, 28 208 severe cases, and 1823 deaths (CFR 0.06).
DENV is the most widespread arbovirus and causes the highest number of arboviral disease cases in the Region of the Americas, with cyclic epidemics recurring every 3 to 5 years. Approximately 500 million people in the region are at risk of dengue infection today. Ae. aegypti, the vector mosquito for dengue, is widely distributed in the Americas, only Canada is free from dengue and its vector. In Uruguay, where Ae. Aegypti is present, limited autochthonous transmission was last reported in 2016, and only imported cases have been reported since then.
All four DENV serotypes (DENV-1, DENV-2, DENV-3 and DENV-4) are currently circulating in the Americas. DENV-3 and DENV-4 are being detected more frequently in 2023 after several years of predominant detection of DENV-1 and DENV-2. Nevertheless, nine countries are reporting the co-circulation of all four dengue serotypes. Simultaneous circulation of all these serotypes has been detected in Brazil, Colombia, Costa Rica, Guatemala, Honduras, Mexico, Nicaragua, Panama, and Venezuela. The Arbovirus Diagnosis Laboratory Network of the Americas (RELDA as per its acronym in Spanish) has been strengthened to face the introduction of new dengue serotypes and the re-emergence of other arboviral diseases, such as chikungunya, Zika, and West Nile virus, all of which are currently circulating in the region alongside dengue. The main objective of the network is to ensure efficient laboratory surveillance and robust installed capacity to respond to outbreaks and epidemics.
WHO Eastern Mediterranean Region:
Dengue and severe dengue epidemics were first reported in the Region in 1998, and since then, their frequency and geographical spread have increased, with outbreaks occurring in all nine endemic countries: Afghanistan, Djibouti, Egypt, Oman, Pakistan, Saudi Arabia, Somalia, Sudan, and Yemen.
Among these are fragile, conflict affected and vulnerable countries such as Afghanistan, Pakistan, Sudan, Somalia and Yemen. The outbreaks are exacerbated due to disruption of health services (Sudan), fragile health systems (Afghanistan, Somalia, Sudan, Pakistan and Yemen), mass population movements, poor water and sanitation infrastructure, and recurring natural disasters such as floods affecting Somalia, Sudan, Pakistan, and Yemen, along with earthquakes in Afghanistan. Outbreaks are also reported in middle- and high-income countries such as Egypt, Oman and Saudi Arabia due to climate change leading to unusual rainfalls. Pakistan (n= 20 072), Saudi Arabia and Oman have reported the highest number of confirmed cases thus far in 2023.
During these epidemics, all four serotypes of dengue virus were known to circulate in the Region. Ae. aegypti is the predominant and primary vector transmitting dengue in the EMR endemic countries. More recently, Bahrain, Iran, and Qatar have reported the presence of Ae. aegypti, although no local transmission of dengue has been documented. Additionally, presence of the secondary vector of dengue, Ae. albopictus, has also been reported from ten EMR countries (Afghanistan, Iran, Jordan, Lebanon, Morocco, Oman, Pakistan, Palestine, Syria and Tunisia).
The effectiveness of response measures is hindered by several factors including i) constrained laboratory capacities ii) challenges in accessing healthcare iii) shortages of human resources iv) limited and inconsistent vector surveillance v) insecticide resistance, vi) poor community engagement and health education vii) a fragmented surveillance system. vii) The ongoing armed hostilities in many Eastern Mediterranean Region countries further compound the complexities of response efforts.
WHO European Region:
Dengue is not endemic in the WHO European Region and cases are mainly travel-related; however, since 2010, there have been reports of autochthonous cases in a number of countries in the region, including Croatia, France, Israel, Italy, Portugal and Spain. In 2018, the year with the most comprehensive data available, a total of 2500 cases of dengue were reported to WHO through the regional annual surveillance data collection mechanism with Germany, France, and the United Kingdom contributing the majority of cases. The vast majority of these cases were imported. However, it should be noted that data completeness remains challenging.
Between 1 January and 5 December 2023, sporadic autochthonous cases and outbreaks have been reported in three countries: Italy (n = 82), France (n = 43) and Spain (n = 3). Routine testing for dengue in Member States of the WHO European Region is not common unless there is a travel history and clinical suspicion, hence the actual numbers of dengue cases in 2023 is likely to be underestimated. One death of an imported, travel-related case was reported in Italy; no additional deaths have been reported in European countries in 2023 to date.
The Ae. albopictus mosquito, which is the main vector of dengue virus in Europe, is established in several Southern European countries. Ae. albopictus mosquitoes have been detected further north and west in the past ten years and it has capacity to hibernate in winter. In 2023, this mosquito species has been identified in 13 countries of the region, a notable increase from eight countries in 2013.
While cold winters prevent year-round transmission of mosquito-borne diseases, the climatic suitability for transmission of DENV in Europe is increasing, leading to floods and stagnant water pools. These create more favorable conditions for the competent vector population. Ae. aegypti (principal dengue vector in most countries) does not survive over winter well but has been established in Cyprus and Madeira, Portugal since 2022.
These trends can potentially lead to an increase in the number of dengue cases and possible fatalities.
Robust public health systems in many countries, including access to early diagnosis, case referral, and management of severe cases, contribute to reduced severe health impact and further disease spread for both imported and autochthonous cases.
WHO South-East Asia Region:
In the WHO Southeast Asia region, 10 out of 11 Member States are known to be endemic for dengue virus. In 2023, several countries, including Bangladesh and Thailand, have reported a notable surge in dengue cases compared to previous years. In particular, India, Indonesia, Myanmar, Sri Lanka and Thailand rank among the world’s 30 most highly endemic countries.
Compared to 2022, in 2023, Bangladesh and Thailand recorded a larger number of dengue cases . By November 2023, Bangladesh experienced a substantial rise in cases reaching 308 167 compared to 62 382 reported for the entirety of 2022. Thailand saw an increase of over 300%, with dengue cases rising from 46 678 in 2022 to 136 655 in 2023 (as of 22 November 2023). During the same period, the death toll in Bangladesh rose from 281 (CFR 0.45%) to 1598 (CFR 0.52%), while in Thailand, it increased from 34 (CFR 0.07%) to 147 (CFR 0.11%). In other countries, the CFR ranged from 0.04% in Nepal to 0.72% in Indonesia. It’s important to interpret these values cautiously due to variations in the case definition used across countries, with some systems primarily focused on reporting hospitalized or severe dengue cases.
In addition, spatial and temporal shifts in dengue patterns were observed in 2022 and continued in 2023. Nepal and Bangladesh experienced spikes in case numbers earlier than usual. Cases in Nepal shifted from the Kathmandu Valley in 2022 to the southeast Terai region and hill districts in Gandaki province in 2023. India, in 2023, experienced an increase in cases in Kerala and northeastern States bordering Bangladesh compared to the previous year.
WHO Western Pacific Region:
The Western Pacific Region continues to face a high burden of mosquito-borne arboviral diseases, particularly dengue. These diseases cause significant morbidity and mortality, especially among those unreached by quality primary health care (PHC) services.
Between 1 January 2023 to 7 December 2023, over 500 000 dengue cases and 750 deaths were reported from eight countries/territories/areas in the WHO Western Pacific Region: Australia, Cambodia, China, Lao People’s Democratic Republic, Malaysia, Philippines, Singapore, and Viet Nam. The most affected countries are the Philippines, reporting 167 355 cases and 575 deaths (CFR 0.34%), and Viet Nam with 149 557 cases and 36 deaths (CFR: 0.02%). Dengue is endemic in several countries such as Cambodia, Lao People’s Democratic Republic, the Philippines, and Viet Nam.
In Pacific Island countries/territories (n = 21), in 2023, dengue-like illness1 was reported from nine Pacific countries/territories, resulting in a total of 13 339 cases, a 28% increase reported as of 30 November compared to 2022. Among the most affected are Fiji, which reported 8418 cases in 2022 and 11 522 cases and 2023, reflecting a 37% increase.
Member States with endemic transmission continue to report longer seasonal dengue epidemics with increasing magnitude and geographic spread. However, disease incidence is less reliable due to the underreporting of cases, particularly in the Pacific Island Countries and territories based on their current syndromic surveillance of dengue as dengue-like illness (DLI) reporting system. Furthermore, the reported number of deaths due to severe dengue is variable. As such, country-level and sub-national case fatality rates (CFR) may appear inconsistent.
Due to the endemicity of dengue and public health burden in the Western Pacific Region, in 2008, the Regional Committee for WPR endorsed the Dengue Strategic Plan for the Asia Pacific Region 2008-2015 (resolution WPR/RC59.R6), serving as a road map. Subsequently, in 2016, considering the growing regional trends in dengue morbidity and mortality, the Western Pacific Regional Action Plan for Dengue Prevention and Control was developed. This plan recommended a switch in strategy from outbreak containment to reducing the impact of dengue on communities. There is a window of opportunity for Pacific countries/territories to improve the adherence to the existing WHO “Framework for National Surveillance and control plans for Aedes vectors” in the Pacific for non-endemic countries in the Pacific Region. Given the impact of climate change on the spread and endemicities of Arboviral diseases, establishing a comprehensive Early Warning System (EWS) that integrates climate, disease, viral/ serological, and entomology surveillance is crucial. Such a system has the potential to predict future risks in vulnerable communities.
Epidemiology
Dengue virus (DENV) is transmitted to humans through the bite of infected mosquitoes typically in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. The primary vectors that transmit the disease are Aedes aegypti and, to a lesser extent, Aedes albopictus mosquitoes, though in some regions such as Europe and North America this latter vector is more widespread.
DENV has four serotypes (DENV-1, DENV-2, DENV-3, DENV-4). Infection with one serotype provides long-term immunity to the same serotype and only transient immunity to the other serotypes, after which secondary infections with a different serotype increase the risk for severe dengue. Dengue cases are most commonly asymptomatic or result in mild febrile illness. However, some cases will develop severe dengue, which may involve shock, severe bleeding or severe organ impairment. This stage often starts after the fever has gone away and it is preceded by warning signs such as intense abdominal pain, persistent vomiting, bleeding gums, fluid accumulation, lethargy or restlessness, and liver enlargement.
There is no specific treatment for dengue, but the timely diagnosis of dengue cases, identification of warning signs for severe dengue, and appropriate clinical management are key elements of care to prevent the progression to severe dengue and deaths.
Public Health Response
Heterogeneity in capacity across Member States impacts the ability to detect and respond to DENV endemic and epidemic transmission. While the majority of the countries in the Americas, South-East Asian and Western-Pacific regions are endemic for the disease and have the capacity to manage cases, a few countries do not mandate reporting of dengue cases and thus under- or non-reporting of cases results in pockets of vulnerability within regions. Simultaneous outbreaks across multiple WHO regions strain the capacity for epidemic response. The overall capacity to respond to multiple, concurrent outbreaks continues to be strained due to the global lack of resources, including shortages of good quality dengue diagnostic kits for early detection, lack of trained clinical and vector control staff, and lack of resources to support risk community and community engagement interventions. Prevention and control of dengue continue to be variable due to changes in the predominant circulating serotypes and co-circulation of multiple dengue serotypes in the different regions, limited funding, competing health priorities and diverse perceptions about the effectiveness of interventions and control measures. Surveillance and response capacity is particularly limited in many countries in the African region, and as stated earlier, five of the Eastern Mediterranean Member States with DENV are dealing with conflicts and natural disasters.
There is a pressing need to increase advocacy and resource mobilization in an integrated approach to influence policymakers in affected countries within these regions.
The following activities are being undertaken at WHO to support Member States in the response to this event.
- Coordination and leadership
- Establishment of a Global Joint Incident Management Support Team (IMST) at WHO, involving WHO Health Emergencies Programme (Response and Preparedness departments) and technical expertise from the Neglected Tropical Disease department to support the response to outbreaks.
- Implementation of integrated response aligned with the overarching Global Arbovirus Initiative. The Global Arbovirus Initiative is an integrated strategic plan to tackle emerging and re-emerging arboviruses with epidemic and pandemic potential focusing on monitoring risk, pandemic prevention, preparedness, detection and response, and building a coalition of partners. The initiative is a collaborative effort between the World Health Emergencies Programme, the Department of Control of Neglected Tropical Diseases, and the Immunization, Vaccines and Biologicals Department. This integrated initiative will build a coalition of key partners to strengthen the coordination, communication, capacity-building, research, preparedness, and response necessary to mitigate the growing risk of epidemics due to these diseases.
- Preparedness and Response
- Conducting risk mapping to categorize countries (preparedness, readiness or response) and to enable appropriate packages of interventions to be developed.
- Developing global operational response plan and a strategic plan for preparedness and response including needs and required funds.
- Supporting Member States through the development of guidelines on preparedness and response to dengue outbreaks (including the strengthening of epidemiological and entomological surveillance, laboratory diagnosis and genomic surveillance, clinical management, risk communication and community engagement (RCCE), vector surveillance and control, and also organization of health services).
- Provision of technical support to all ongoing outbreaks (epidemiology, laboratory, case management, RCCE including behavioral science, and vector and environmental surveillance and control.
3.Multisectoral collaboration
- Support country adoption of a multisectoral One health strategy while preparing for and responding to dengue outbreaks as well as other arboviral diseases.
- Collaboration with One Health and climate change partners to coordinate the multisectoral response to dengue outbreaks.
- Supporting the deployment of experts through GOARN and Standby Partners to countries that are experiencing high-magnitude outbreaks.
- Vector control activities
- Supporting the implementation of effective integrated vector management (surveillance and control) by Member States (in priority countries) through publishing guidelines and the provision of epidemiological surveillance materials and technical assistance to national authorities.
- Working with Member States to support the vector control response with specialized vector control technicians to help coordinate the response.
- Support training on insecticide resistance management and vector surveillance in Member States.
- Laboratory
- Support the strengthening of laboratory-capacity to enable timely and accurate diagnosis and case detection in affected and at-risk countries.
- Leveraging the capacities built during the COVID-19 pandemic to strengthen molecular diagnosis and genomic surveillance at the country level.
6. Operations, Support and Logistics (OSL)
- Working closely with suppliers to secure dengue kits and establishing a pipeline for bulk items.
- Supporting Member States in purchasing equipment and insecticides and provision of insecticide resistance management kits.
- Case management guidelines and capacity building
- Sharing case management guidelines and clinical training with health care workers through webinars and refresher sessions.
- Ongoing development of the WHO guideline for the clinical management and diagnosis of dengue, chikungunya, Zika, and yellow fever, due for completion in early 2024, which will be an important tool.
- WHO/PAHO has produced a 20-hour self-learning, virtual course on dengue clinical management, available in Spanish and English languages, focused on identifying early predictors of severe disease (warning signs) and preventing the progression of dengue cases to severe dengue and deaths. The course has already trained over 312 000 clinicians since its launch in September 2020 (219 000 in 2023 alone).
- Epidemiological Surveillance
- Virtual cooperation spaces (VCS) have been created for collaborative surveillance between PAHO and its Member States that allow the automated generation of different epidemiological analyses, situation rooms, and epidemiological bulletins, strengthening the epidemiological surveillance of dengue and other arboviruses.
- In 2023, PAHO/WHO issued five updates on the dengue situation in the Region of the Americas and an epidemiological alert regarding the increase in dengue cases in Central America and the Caribbean.
- The WHO Regional Office for Africa has developed a country risk classification tool for dengue, which is being adapted for use in other regions.
- WHO is working globally to enhance surveillance for dengue cases, severe dengue, and dengue deaths, in order to better understand the global burden in a more timely manner.
- Risk communication and community engagement (RCCE)
- Providing advice on risk assessment, including community centered approach.
- Supporting the development of RCCE evidence based and tailored interventions, encouraging both Individual and community actions.
- Reviewing existing RCCE materials and lessons learned from previous and ongoing outbreaks.
- Finalizing the RCCE toolkit on dengue.
WHO Risk Assessment
Recent data from 2023 emphasize escalated dengue outbreaks in several countries, particularly Bangladesh, Brazil, Burkina Faso, Fiji, Pakistan, the Philippines, and Viet Nam. Additionally, non-endemic countries are increasingly facing dengue as a significant public health concern. The emergence and re-emergence of dengue and its unprecedented worldwide spread are linked to various factors: i) Changing distribution and adaptation of the Aedes aegypti vector; ii) increased unplanned urbanization and human activities fostering conducive environments for vector-host interaction; iii) Climate change-induced shifts in weather patterns; iv) Fragile healthcare systems amidst political and financial instabilities; v) Co-circulation of multiple dengue serotypes; vi) Challenges in clinical diagnosis due to non-specific symptoms; vii) Inadequate laboratory and testing capacity; viii) Prolonged ongoing concurrent outbreaks, including COVID-19; ix) Lack of specific treatment for dengue; x) Limited behavioral data available on community risk perceptions, awareness and health seeking behaviors: xi) Lack of community centered approach and RCCE resources to support engagement and mobilization of local communities in vector control activities; xi) Insufficient vector surveillance and control capacities and, xii) Lack of coordination among stakeholders, chronic underfunding, low donor interest and xii) large scale movement of people and goods.
The expansion of DENV beyond its endemic transmission areas presents additional challenges. A significant population that is immunologically naïve to the current virus circulating, increasing the risk of outbreaks. Moreover, people in these areas might lack awareness of dengue warning signs, leading to potential delays in seeking health care which is critical to reducing mortality from severe disease. Accessibility challenges to medical facilities, compounded by limited geographical access, heighten the difficulty in accessing basic healthcare services. These challenges are aggravated by stockouts of essential supplies for prevention and control, laboratory diagnostic reagents, and the need for ongoing training of healthcare workers.
These factors, along with others, including financial crises, mass migration of internally displaced persons (IDPs) and refugees, and longstanding developmental inadequacies, have deprived large populations across all continents of adequate healthcare, consequently increasing their vulnerability to dengue. However, it is important to note that the distribution of dengue risk varies significantly across regions, countries, and within countries.
Based on all the above WHO has assessed the risk at global level as high. Following the risk assessment and an internal grading process, WHO Regional Offices have agreed on priority interventions to implement in support of Member States.
Dengue prevention and outbreak response involves several agencies in the public health sector. Addressing these challenges requires a multidisciplinary and multisectoral integrated approach, especially at national level to achieve its goal of reducing the impact on public health. The strain on epidemic response capacity due to simultaneous concurrent outbreaks coupled with political crises highlights the need for robust emergency response mechanisms and strengthened collaboration among stakeholders. The global lack of resources, including shortages of good quality dengue diagnostic kits for early detection, lack of trained clinical and vector control personnel, and community awareness remain a critical obstacle to an effective response. While coordination efforts with global health organizations like WHO and other partners strive to set common priorities and analyses, the need for continuous support to affected countries and enhanced collaboration is imperative.
WHO Advice
Effective vector control measures:
Effective vector control is key to the prevention and control of the DENV. Vector control activities should target all areas where there is a risk of human-vector contact, such as residences, workplaces, schools, and hospitals. WHO promotes Integrated Vector Management (IVM) to control Aedes species. IVM should include removing potential breeding sites, reducing vector populations, and minimizing individual exposure. This should involve vector control strategies for larvae and adults (i.e., environmental management and source reduction), especially monitoring water storage practices, draining and cleaning household water storage containers weekly, larvicide in non-potable water using WHO-prequalified larvicides at correct dosages, distribution of insecticide-treated nets (ITNs) for fever/dengue inpatients to contain spread of the virus from health facilities. Indoor space spraying for rapidly containing dengue-infected mosquitoes may be challenging to deliver in densely populated areas.
The Global Arbovirus Initiative promotes coordination and collaboration among multisectoral partners, an integrated vector management approach and sustained control measures at all levels. Its guiding principle is to harmonize prevention, surveillance (entomological and epidemiological) and case management with existing health systems, such that they are sustainable, cost-effective and ecologically sound.
Personal Protective Measures:
Personal protective measures during outdoor activities include topical repellents to exposed skin or the treatment of clothing and using long-sleeved shirts and pants. Additionally, indoor protection can include the use of household insecticide aerosol products, or mosquito coils during the day. Window and door screens can reduce the probability of mosquitoes entering the house. Insecticide-treated nets offer good protection to people against mosquito bites while sleeping during the day. Since Aedes mosquitoes are most active at dawn and dusk, personal protective measures are recommended particularly at these times of day. Personal protection measures and mosquito control should also cover workplaces and schools since the vectors are day-biting mosquitoes.
Entomological Surveillance:
Entomological surveillance should be undertaken to assess the breeding potential of Aedes mosquitoes in containers and monitor insecticide resistance to help select the most effective insecticide-based interventions.
Case management:
There is no specific treatment for dengue infection. However, early detection and access to appropriate healthcare for case management can reduce mortality, as can rapid detection of severe dengue cases and timely referrals to tertiary healthcare facilities.
Most people with dengue have mild or no symptoms and will get better in 1–2 weeks.
Individuals who are infected for the second time are at greater risk of severe dengue. Severe dengue symptoms often come after the fever has gone away such as:
- severe abdominal pain
- persistent vomiting
- rapid breathing
- bleeding gums or nose
- fatigue
- restlessness
- blood in vomit or stool
- being very thirsty
- pale and cold skin
- feeling weak.
People with these severe symptoms should get care right away.
Enhanced case surveillance:
Case surveillance should be enhanced in all affected countries and globally. Where feasible, resources should be allocated for the strengthening of surveillance to determine the overall dengue burden (i.e., including outpatient cases), counting severe and fatal cases, and for the confirmation and sub-typing of the dengue virus.
Operational research and learning from successful examples:
Countries must learn and adopt successful examples of effective case management, prevention, community engagement, and vector control of dengue and other arboviruses through heightened research projects, particularly given the recent WHO recommendations on clinical trials.
Ministries of Health and partners should closely review local interventions to accept and recommend them for public health programmes for early adaptation to reduce the growing health impact of dengue.
WHO does not recommend that any general travel or trade restrictions be applied to countries/territories/areas based on the available information.
Further Information
- WHO Fact sheet: Dengue and severe dengue
- Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021–2030
- Public Health Situation Analysis: El Niño (October-December 2023)
- Establishing syndromic surveillance and event-based surveillance systems for Zika, dengue and other arboviral diseases;
- Half of world population at risk of dengue virus : WHO
- WHO warns of dengue risk as global warming pushes cases near historic highs
- Laboratory testing for Zika virus and dengue virus infections
- Dengue and severe dengue cases and deaths for the subregions of the Americas
- PAHO dengue situation reports
- PAHO Guidelines for clinical diagnosis and treatment of dengue, chikungunya and zika (2022)
- Dengue situation in America
- ECDC, increasing risk of mosquito-borne diseases in EU/EEA following spread of Aedes species
- Vector control: the ARS confirms a first indigenous case of dengue in Île-de-France and initiates two mosquito control actions in Limeil-Brévannes (94)
- Dengue cases in Italy: updated data
- WHO Bangladesh. Dengue Situation Report, Issue # 10, 30 Oct 2023
- Disease Outbreak News. Dengue – Bangladesh
- National Dengue Control Unit, Ministry of Health. Publications, 2023
- Western Pacific regional action plan for dengue prevention and control (2016)
- WPRO dengue situation reports
1DLI (Dengue Like Illness). Case definition: Fever for at least 2 days, in addition to at least two of the following:
i. Nausea or vomiting; ii. Muscle or joint pain; iii. Severe headache or pain behind the eyes; iv. Rash;v. Bleeding
Citable reference: World Health Organization (21 December 2023). Disease Outbreak News; Dengue – Global situation Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON498