Clinicians grappling with long COVID confront a significant hurdle—diagnosing and acknowledging the condition lacks consensus. However, a recent study suggests that specific biomarker testing could pinpoint long COVID with an accuracy nearing 80%.
Accurate diagnosis holds immense potential in the battle against long COVID. It extends beyond the persistent symptoms like fatigue, brain fog, and heart palpitations; it encompasses mental health struggles, with two-thirds of long COVID patients contending with depression or anxiety. Many patients lament their symptoms being dismissed by doctors, while up to 12% face unemployment due to the severity of their illness, often met with skepticism by employers.
Swift and precise diagnosis could change this narrative. A new preprint study proposes that the elevation of certain immune system proteins may serve as a reliable diagnostic indicator for long COVID.
Researchers from Cardiff University School of Medicine in the UK monitored 166 recovered COVID patients, distinguishing between 79 with long COVID and 87 without. Analyzing their blood plasma revealed heightened levels of specific components. Notably, four proteins—Ba, iC3b, C5a, and TCC—predicted long COVID presence with 78.5% accuracy.
Lead researcher Wioleta Zelek, PhD, expressed astonishment at these findings, citing a significant dysregulation in these biomarkers, showcasing their predictive value for long COVID.
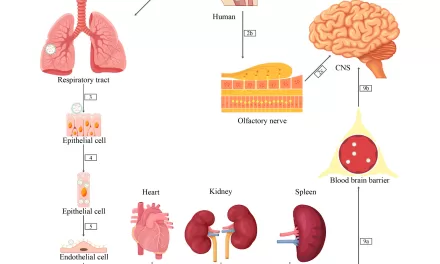
The study unveiled that long COVID associates with immune system inflammation, leading to sustained dysregulation of these complement proteins. While the symptoms of long COVID may seem disparate, elevated inflammation emerges as a common thread, causing systemic disturbances in the body.
Nisha Viswanathan, MD, from UCLA Health, lauds any research aiding in long COVID diagnosis within the clinical community. Biomarker testing, including those highlighted in the study and others like serotonin and cortisol, may aid in differentiating long COVID from similar symptomatic conditions.
Viswanathan warns that while biomarker testing is promising, it doesn’t address all diagnostic queries. For instance, the study doesn’t clarify if complement dysregulation stems specifically from long COVID or pre-existing conditions in patients.
Researchers increasingly view long COVID as an umbrella term for diverse conditions triggered by varied virus impacts. Further investigations delve into different long COVID phenotypes, hinting at distinct disease mechanisms for different symptom clusters.
Enhanced diagnostics pave the way for better treatments. Understanding the immune dysregulation mechanisms in long COVID may enable doctors to employ existing medications effectively. Drugs like pegcetacoplan and zilucoplan, initially approved for other conditions, show promise in alleviating inflammation and reducing long COVID symptoms.
While the Cardiff University study provides detailed insights into long COVID biomarkers, infectious disease specialist Grace McComsey emphasizes the need for broader studies involving multiple biomarkers to corroborate findings. The aim is to consolidate these puzzle pieces into common diagnostic tools, providing patients a clearer path toward recovery.