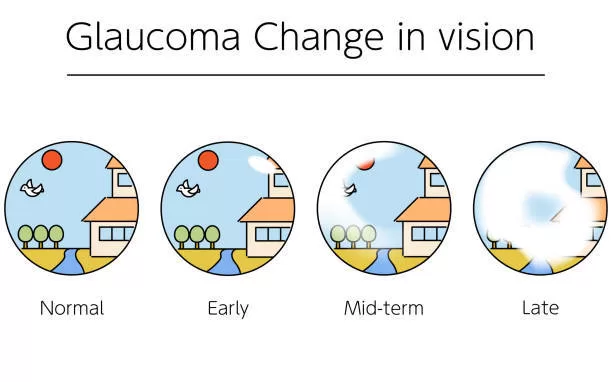
A stealthy ailment is on the rise among the elderly globally, with millions unknowingly grappling with glaucoma—an eye condition capable of causing irreversible blindness, yet exhibiting no obvious symptoms until the disease reaches an advanced stage, caution ophthalmologists.
Projections indicate that by 2050, the number of individuals affected by glaucoma will surge by over 200%, underscoring the pressing need for heightened awareness, early detection, and advanced treatment approaches.
Dr. Joel S. Schuman, a professor of ophthalmology and co-director of the Glaucoma Service at Wills Eye Hospital in Philadelphia, remarked, “That’s a significant number of individuals with a debilitating condition who are unaware of their affliction. In the late stages of the disease, people might notice stumbling over curbs or bumping into objects they didn’t see. It’s really only in very advanced stages that people become aware that something is amiss.”
Glaucoma ranks as the second leading cause of blindness globally, impacting three million individuals in the United States. Shockingly, half of those affected remain unaware, according to the CDC.
Recent research conducted at the University of Gothenburg in Sweden underscores the insidious nature of glaucoma: 5% of 560 seventy-year-olds had the disease, and half of them were unaware prior to participating in the study.
Lena Havstam Johansson, a PhD student at the University of Gothenburg and a specialist nurse at Sahlgrenska University Hospital, who conducted the study, stated, “Living with glaucoma, especially without realizing it, can be very isolating. It may lead people to stay at home to avoid the trouble.”
When symptoms do manifest, some individuals may observe patchy blind spots in their peripheral or central vision in advanced stages. However, many people mistakenly attribute these changes to age-related clumsiness, when in fact, they may have a condition that can be slowed with the appropriate treatment.
Glaucoma arises from increased pressure within the eye, leading to damage to the optic nerve, which transmits visual information to the brain. Without intervention, it progresses to partial or complete vision loss. Its gradual onset and lack of early symptoms have earned it the moniker “the silent thief of sight.”
While various forms of the disease exist, about nine out of ten cases in the U.S. are of the primary open-angle glaucoma (POAG) variety.
It primarily affects those over sixty, individuals with a family history of glaucoma, and those with diabetes. It disproportionately affects Black individuals, who are six times more likely than White individuals to experience advanced vision loss from the disease.
In the U.S., over 120,000 people are blind due to glaucoma, constituting 9% to 12% of all blindness cases.
Treatment options for glaucoma range from eyedrops to laser procedures to surgical interventions, all aiming to reduce intraocular pressure. Some doctors may recommend oral medication in addition to eyedrops. “We have a lot of treatment options, and they work pretty well,” remarked Dr. Schuman. “But the first step is the person knowing they have glaucoma, and the second step is that person seeking care.”
Less common types of glaucoma include normal-tension glaucoma, more prevalent among individuals of Japanese ancestry, and congenital glaucoma, which is present from birth and affects approximately one in 10,000 babies born in the U.S.
To ensure early detection and treatment, regular eye exams are crucial—every two to four years for adults under fifty-five, and annually thereafter, advised Dr. Annie Wu, a clinical assistant professor of ophthalmology at the Kellogg Eye Center at the University of Michigan.
The slow development of glaucoma symptoms, coupled with limited access to eye specialists faced by many Americans, amplifies the danger posed by the disease.
The University of Pennsylvania is among those working to address this issue, hosting free glaucoma screening programs for Black residents. Black Americans are five to six times more likely to receive a glaucoma diagnosis, as per the school’s statement.
Numerous organizations also offer access to free glaucoma screening.
Glaucoma testing can be incorporated into routine eye exams and may involve one or a combination of relatively quick and painless tests. These may encompass dilating the pupil with eyedrops to examine the optic nerve, as well as measuring corneal thickness to determine risk, which is higher with thinner corneas.
Dr. Wu emphasized, “It is important not to wait until you have symptoms. If glaucoma has progressed to the point where you’re noticing it in your central vision, it means you’ve lost most of your peripheral field. Definitely go see an eye doctor, regardless of your family history.”
Source: American Journal of Ophthalmology: “The Changing Face of Primary Open-Angle Glaucoma in the United States: Demographic and Geographic Changes from 2011-2050.”