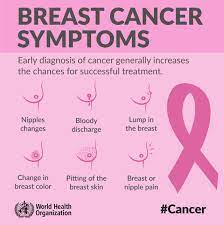
Breast cancer screening is a crucial defense against this deadly disease, yet it grapples with its own set of challenges. While it does lower breast cancer-related fatalities, it also has the potential to detect non-threatening tumors (resulting in overdiagnosis), leading to unnecessary treatments. This not only negatively impacts some women but also unnecessarily escalates healthcare expenses. The concept of ‘risk-based screening’ is a strategy that aims to tailor screening methods based on an individual’s risk profile, with the goal of maximizing benefits while minimizing drawbacks. Customizing screening programs according to individual risks was recently identified as a means to fine-tune screening approaches.
At present, most risk-based breast screening models estimate a woman’s risk of being diagnosed with breast cancer. However, not all instances of breast cancer are lethal, and the risk of diagnosis doesn’t always correlate with the risk of post-diagnosis mortality. Now, researchers have devised a new model that accurately forecasts a woman’s probability of both developing and succumbing to breast cancer within a decade.
This novel model, developed by a team of researchers at the University of Oxford (Oxford, UK), predicts a woman’s combined 10-year risk of both breast cancer development and subsequent mortality. The objective is to identify women at the highest risk of deadly cancers in order to enhance the effectiveness of screening programs. Such high-risk individuals might be encouraged to initiate screening earlier, receive more frequent screenings, or undergo different types of imaging. This personalized approach not only has the potential to reduce breast cancer fatalities but also to spare women with lower risk from unnecessary screening. Women with an elevated risk of deadly cancer could also be considered for preventive treatments against the development of breast cancer.
The research team explored four distinct modeling techniques to predict breast cancer mortality risk. Two followed conventional statistical methodologies, while the other two leveraged machine learning, a branch of artificial intelligence. All models incorporated identical data types, including age, weight, smoking history, family history of breast cancer, and hormone therapy (HRT) usage. The models underwent evaluation for their overall predictive accuracy, spanning various women’s groups with diverse characteristics such as different age brackets and ethnic backgrounds. An approach known as ‘internal-external cross-validation’ was employed. This method involves dividing the dataset into structurally distinct segments, based on factors like region and time frame, to assess the model’s adaptability across different scenarios. The results revealed that a statistical model constructed using ‘competing risks regression’ outperformed the others. This model demonstrated the highest accuracy in predicting which women would develop and face breast cancer mortality within a 10-year span. The machine learning models displayed comparatively lower accuracy, particularly for diverse ethnic women’s groups.
“This is an important new study which potentially offers a new approach to screening. Risk-based strategies could offer a better balance of benefits and harms in breast cancer screening, enabling more personalized information for women to help improve decision making,” said University of Oxford Professor Julia Hippisley-Cox. “Risk based approaches can also help make more efficient use of health service resources by targeting interventions to those most likely to benefit.”