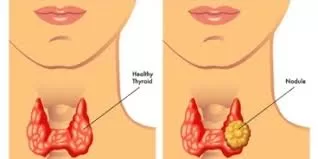
A multicenter phase II clinical trial, led by the University of Chicago Medicine Comprehensive Cancer Centre, has yielded significant insights into the treatment of differentiated thyroid cancer (DTC), which originates from thyroid follicular cells. The study, published in Annals of Oncology on May 13, 2023, examined the potential benefits of combining an immunomodulatory agent with the targeted tyrosine kinase inhibitor (TKI) cediranib, a treatment approach.
While the majority of DTC patients respond well to standard treatments like surgery, hormone therapies, chemotherapy, and radioactive iodine therapy, a small percentage experience cancer recurrence or metastasis, rendering these conventional therapies ineffective. In recent years, there has been growing interest in using TKIs that target vascular endothelial growth factor receptor (VEGFR) signaling in the tumor microenvironment. These TKIs, which inhibit angiogenesis (the formation of new blood vessels), play a crucial role in the progression of thyroid cancer.
To investigate the safety and efficacy of cediranib, a TKI targeting multiple VEGFRs, and its potential synergy with the immunomodulatory agent lenalidomide, oncologists Ari Rosenberg, MD, and Everett Vokes, MD, initiated the study. Lenalidomide is known to block angiogenesis and exhibit anti-tumor properties in various cancers. Previous clinical trials had shown promise in using such combination therapies, which blend traditional treatments with immunotherapies, in treating multiple cancer types.
The phase II clinical trial enrolled 108 patients from various medical centers in the United States and Canada, randomly assigning them to one of two treatment groups: cediranib alone (39 patients) or cediranib with lenalidomide (69 patients). The results revealed that the cediranib alone group achieved a median progression-free survival (PFS) of 14.8 months, with 44% of patients experiencing complete or partial tumor disappearance (objective response rate, ORR).
Unexpectedly, the addition of lenalidomide to cediranib did not yield superior outcomes compared to cediranib treatment alone. This finding contrasted with previous successes of combining VEGF-targeted TKIs with immunotherapeutic strategies in other cancer types, such as renal cell carcinoma and hepatocellular carcinoma. The study emphasized the importance of randomized trial designs, as single-arm studies can sometimes produce misleading positive results. It also highlighted that immunomodulation has not proven effective thus far in treating thyroid cancer.
In conclusion, the study affirmed that cediranib is an active agent, with ORR and PFS outcomes similar to other approved VEGFR-targeted TKIs in DTC, including lenvatinib, sorafenib, and vandetanib. However, it underscored the limitations of combining lenalidomide, an immunomodulatory agent, with VEGFR-targeted TKIs in this specific context. The research suggests a need to explore new combinations and mechanisms, particularly innovative immunotherapeutic strategies, to improve outcomes for thyroid cancer patients. Despite the study’s enrollment of patients from 2010-2015, its findings remain relevant, as no significant improvements have occurred beyond single VEGFR-targeted TKIs in the treatment of DTC.