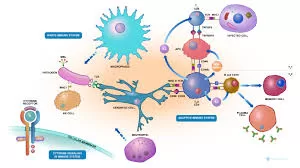
When the immune system of an immunocompromised individual initiates healing and boosts the production of white blood cells, it’s generally considered a positive sign—unless they develop a potentially fatal inflammatory condition. Fresh research conducted by the University of Illinois Urbana-Champaign sheds light on a common respiratory distress linked to this ailment, revealing that it’s not caused by lung damage, but rather by the infiltration of newly activated T-cells into the brain.
Understanding this mechanism can significantly enhance the comprehension of the illness for researchers and medical practitioners, aiding in the identification of novel therapeutic targets. Makoto Inoue, the lead researcher and a professor of comparative biosciences at Illinois, highlights that these findings have been published in the journal Nature Communications.
This specific condition, termed Cryptococcus-associated immune reconstitution inflammatory syndrome (CIRIS), emerges when an immunocompromised patient unknowingly contracts the Cryptococcus fungus. As the patient’s immune system begins to rebuild and generate more T-cells, the infection triggers widespread inflammation. CIRIS commonly affects patients undergoing antiretroviral therapy, recovering from chemotherapy, transplants, and it’s also been observed in postpartum women and those with multiple sclerosis. However, diagnosing CIRIS remains challenging, often necessitating the elimination of other potential causes as a preliminary step, according to Jinyan Zhou, a graduate student researcher at Illinois and a co-author of the study.
To delve deeper into the condition and its progression, the research team developed a mouse model of the disease. They achieved this by administering T-cell injections to immune-deficient mice already infected with Cryptococcus, simulating the process that occurs when the immune system rebounds with heightened T-cell levels following suppression. The symptoms observed in the mice, including brain inflammation, cerebral fluid accumulation, and pulmonary dysfunction, closely mirrored those found in human patients.
Zhou explains, “We observed a significant influx of T-cells into the brains alongside pulmonary dysfunction, suggesting a potential connection between the two. Under normal circumstances, the brain shouldn’t house such a large number of T-cells, as they are primarily distributed in peripheral areas with only a limited number of T-cells responsible for brain surveillance.”
Delving further into their investigation, the researchers unraveled a sequence of events that lead to T-cell infiltration into the brain and subsequent respiratory issues. A receptor known as CCR5, associated with conditions like HIV and cancer, was found on the surface of T-cells and played a pivotal role.
As the T-cell population increased in the mice, the CCR5 receptor facilitated the infiltration of these white blood cells into the brain. Furthermore, the T-cells that successfully infiltrated the brain generated substantial quantities of two molecules known to inflict damage on neurons in the regions controlling respiratory function.
Inoue remarked, “Discovering that the pulmonary dysfunction stems from neuron damage in the brain represents a novel perspective on this condition. While we’re aware of the brain’s influence on various peripheral organs, this insight holds significance for clinicians treating this syndrome. Typically, drugs are administered to enhance lung function, but with limited success. Now, understanding the brain’s role, we have fresh avenues for targeted treatments.”
In order to validate this series of events and identify potential paths for treatment, the researchers treated a set of mice with a drug that suppresses the CCR5 receptor. Notably, both pulmonary function and neuronal development showed improvement.
Zhou adds, “We believe that this approach could be beneficial for C-IRIS patients as well—preventing the infiltration of T-cells into the brain and subsequently averting symptom manifestation. Additionally, we could target the molecules responsible for damaging neurons. For instance, in patients prescribed immunotherapies, we could potentially manipulate these T-cells to reduce the expression of those harmful molecules.”
Moving forward, the research team intends to delve deeper into other facets of the immune system’s role in CIRIS, exploring further interactions between T-cells and various systems within the brain and body.
Source ANI










