Situation at a glance
From 1 January to 7 August 2023, the Ministry of Health and Family Welfare of Bangladesh reported a total of 69 483 laboratory-confirmed dengue cases and 327 related deaths, with a case fatality rate (CFR) of 0.47%. Of these, 63% of cases and 62% of the deaths were reported in the month of July 2023. Although dengue is endemic in Bangladesh, the current dengue surge is unusual in terms of seasonality and the early sharp increase in comparison to previous years, where the surge started around -late June. The CFR so far this year is relatively high compared to previous years for the full-year period. The pre-monsoon Aedes survey shows that the density of mosquitoes, and the number of potential hotspots is at the highest level in the past five years.
The higher incidence of dengue is taking place in the context of an unusual episodic amount of rainfall, combined with high temperatures and high humidity, which have resulted in an increased mosquito population throughout Bangladesh.
Description of the outbreak
Between 1 January and 7 August 2023, a total of 69 483 dengue cases including 327 related deaths (case fatality rate = 0.47%) were reported by the Ministry of Health and Family Welfare (MOHFW). As of 30 June 2023, a total of 7978 cases and 47 deaths were reported, however, the cases started surging rapidly from late June and in the month of July alone 63% of cases (n=43 854) and 62% of deaths (n= 204) were reported.
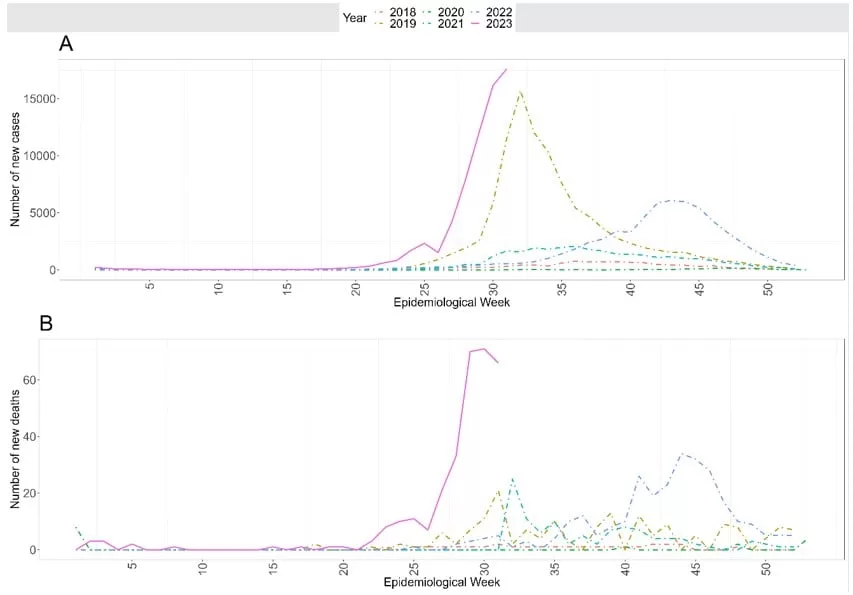
The number of cases and deaths are higher compared to similar periods in the past five years (Figure 1). Dengue cases started to rise in May 2023 and have been continuing since then, and the peak is unlikely to have been reached. The reported number of dengue cases this year is the highest compared to the same periods recorded since 2000.
The cases are reported from all 64 districts in the country. Cases in Dhaka division started to increase in epidemic week 17 (23-29 April 2023) and in all eight divisions since epidemic week 26 (25 June to 1 July 2023). The most affected area in the Dhaka division is Dhaka city corporation, accounting for 52.8% of cases and 78.9% of deaths. Other affected divisions include Chattogram division (13.2% of cases and 9.2% of deaths), Dhaka division excluding Dhaka city (11.6% of cases and 2.8% of deaths), and Barisal division (10.5% of cases and 4.3% of deaths). The Sylhet division has the lowest number of cases (560) and no deaths reported so far.
As of 7 August 2023, the reported CFR is 0.47%, which is higher compared to previous years (table 1). On further analysis, the overall CFR is higher in females than in males (0.72% v 0.32%) with females having four times higher CFR than males among those aged 21-40 years (0.71% vs 0.18%). The older age group recorded a higher CFR compared to the younger age group (1.87% in the age group over 60 years compared to 0.74% in the age group between 41 to 60 years and 0.34% in those aged 40 years and below).
DENV2 was the predominant circulating serotype in Bangladesh until 2018, when it was replaced by DENV3 as the predominant serotype since 2019. However, DENV2 has been identified as the primary circulating serotype in this outbreak, and this may result in more severe dengue infections and hospitalizations as a result of a second infection with a heterologous serotype. Of the 66 serotyped samples in the month of June 2023, DENV2 (51.5%) and DENV3 (43.9%) were identified as the circulating serotypes.
Figure 1. Number of dengue cases (A) and deaths (B) reported by epidemic week from 2018 to 2023 [as of 5 August (epidemiological week 31) 2023]
Table 1: Dengue cases, deaths, and case fatality rate in Bangladesh for 2018, 2019, 2021, 2022 and 2023 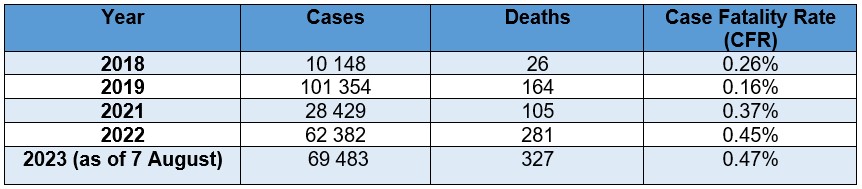
Data source: DGHS (*data for 2020 is limited due to COVID-19)
Epidemiology of dengue
Dengue is a viral infection transmitted to humans through the bite of infected mosquitoes and is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. The primary vectors that transmit the disease are Aedes aegypti mosquitoes and, to a lesser extent, Aedes albopictus.
Dengue virus (DENV) has four serotypes (DENV-1, DENV-2, DENV-3, DENV-4). Infection with one serotype provides long-term immunity to the homologous serotype but not to the other serotypes; sequential infections with a different serotype put people at greater risk for severe dengue. Many DENV infections produce only mild flu-like illness and over 80% of cases are asymptomatic.
There is no specific treatment for dengue; however, the timely detection of cases, identifying any warning signs of severe dengue infection, and appropriate case management are key elements of care to lower case fatality rates to less than 1%.
Dengue was first recorded in the 1960s in Bangladesh (then known as East Pakistan) and was known as “Dacca fever”. Since 2010 cases of dengue appear to coincide with the rainy season from May to September and higher temperatures. Bangladesh’s climate conditions are becoming more favorable for the transmission of dengue and other vector-borne diseases including malaria and chikungunya virus due to excessive rainfall, waterlogging, flooding, rise in temperature and the unusual shifts in the country’s traditional seasons.
Public health response
The high number of reported cases has put pressure on the health systems and the Directorate General of Health Services has taken the following actions:
Coordination
- A coordination committee has been set up under the Director Disease Control & Line Director Communicable Disease Control (CDC) of the Directorate General of Health Services (DGHS) of Bangladesh to oversee the response.
- A Dengue Control Room has been formed (Secretariat) for coordination and data collection at the central level. Additionally, there are Activated Control Rooms in all district and Medical College hospitals.
Health system strengthening for case management:
- Six hospitals assigned for the management of COVID-19 patients in Dhaka city have been repurposed for dengue case management. Additionally, dedicated dengue wards/dengue corners have been established in Medical College hospitals.
- The fourth edition of the National Guideline for Clinical Management of Dengue Syndrome has been updated and instructions were given to all Government and Private Hospitals to follow the guideline.
- There is ongoing capacity building on the clinical management of dengue for doctors and nurses across the country. Pocket guidelines for dengue have been distributed to health care staff.
- Intravenous saline and other supportive medicines, have been supplied to health facilities across the country.
Strengthening surveillance:
- The hospital-based surveillance system is actively collecting regular information from 57 hospitals in Dhaka city as well as all Upazila and district-level hospitals. Daily reports are also disseminated through the Health Emergency Operation Center (HEOC).
Risk communication and community engagement:
- Mass awareness campaigns have been strengthened via television and other mass media methods including digital media, leaflets and posters. Community awareness is also provided by the local ward counsellors. The city corporations have informed all buildings under construction to prevent water collection and fines have been imposed on buildings where the Aedes larvae have been found.
- Advocacy and awareness meetings are ongoing in highly affected wards of Dhaka city corporation by the Aedes Transmitted Disease Control Program and IHR, Migration Health, and Emerging Reemerging Disease Control Program under CDC-DGHS.
Laboratory:
- Dengue serotyping has been conducted.
- A total of 184 000 non-structural protein (NS1) diagnostic kits have been distributed to all Upazila health complexes, district hospitals and medical college hospitals.
Vector control activities:
- The local government engineering department (LGED) is leading vector control activities including the elimination of mosquito breeding sites and larvicidal and adult mosquito control using different insecticides such as Temephos and Deltamethrin.
- Post Monsoon Aedes Survey was carried out in all wards of Dhaka North and Dhaka South city corporation between 26 January 2023 to 4 February 2023. The results were disseminated to concerned stakeholders on 13 April 2023.
- A Pre-Monsoon Aedes Survey started on 18 June 2023 and was completed on 27 June 2023. The results were disseminated to both city corporations on 4 July 2023.
WHO risk assessment
Dengue is endemic in Bangladesh with recurrent outbreaks and is one of the major public health concerns in Bangladesh. Dengue virus has the potential to cause epidemics resulting in high morbidity and mortality.
All four serotypes of the dengue virus have been reported in Bangladesh with the predominance of DENV 1 and DENV2 until 2016. Since 2019, when the largest dengue outbreak was reported, DENV3 has been the predominant serotype, while this year DENV2 has become the predominant serotype.
There is no specific treatment for cases and clinical management is based on supportive therapy however, the early detection of infection and appropriate clinical management of patients can reduce the severity of disease and mortality The prevention and control of dengue depends on vector control.
A dengue vaccine has not been approved in Bangladesh. The dengue risk at the national level is assessed as ‘High’ due to the ongoing rapidly increasing number of cases and deaths with the peak not yet reached, the high CFR compared to the previous years and the increasing geographical distribution of cases. In addition, DENV2 has been identified as the predominant circulating serotype, following four years of DENV3 predominating which may result in higher numbers of severe cases as a result of a second infection with a heterologous serotype. Furthermore, there is some pressure on the healthcare capacity due to the very high number of admissions for dengue; high vector density; and an anticipated prolonged monsoon.
Bangladesh has three international airports, three seaports and twenty-three land ports. Bangladesh shares 94% of its land border with India with frequent population movement across the land crossing, however, dengue is already endemic in India including the eastern Indian states which share land borders with Bangladesh and where Aedes mosquitoes breed and circulate. Climate change along with heavy rains in neighboring countries increase the likelihood of vector-borne disease transmission. Due to social and economic factors, many people migrate from Bangladesh to other countries thereby increasing the risk of international disease spread. Bangladesh receives a large volume of international tourists, and the possibility of travellers acquiring the disease and contributing to its further spread outside the country cannot be ruled out.
WHO advice
The proximity of mosquito vector breeding sites to human habitation is a significant risk factor for dengue virus infection. Aedes species mosquitoes can become infected with the virus after biting DENV-infected individuals and then pass the virus onto other individuals within the vicinity. This cycle, therefore, makes the infective mosquito capable of spreading the dengue virus within households and in the neighbourhood, leading to clusters of cases.
The prevention and control of the DENV, virus that causes dengue, depends on effective vector control. Vector control activities should focus on all areas where there is a risk of human-vector contact such as the place of residence, workplaces, schools, and hospitals. WHO promotes a strategic approach known as Integrated Vector Management (IVM) to control mosquito vectors, including Aedes species, the vector of dengue. IVM should be enhanced to remove potential breeding sites, reduce vector populations, and minimize individual exposure. This should involve vector control strategies for larvae and adults (i.e. environmental management and source reduction, especially of water storage practices, and include covering, draining and cleaning household water storage containers on a weekly basis; larvicide in non-potable water using WHO-prequalified larvicides at correct dosages, distribution of insecticide-treated nets (ITNs) for fever/dengue inpatients to contain spread of virus from health facilities, as well as strategies for protecting people and households. Indoor space spraying (fogging) is another approach for rapid containment of dengue infected mosquitoes but may be challenging to deliver in densely populated areas such as camps.
Personal protective measures during outdoor activities include the topical application of repellents to exposed skin or treatment of clothing, and the use of long sleeves shirts and pants. Additionally, in indoors protection can include the use of household insecticide aerosol products, or mosquito coils during the day. Window and door screens, as well as air conditioning can reduce the probability of mosquitoes entering the house. Insecticide-treated nets offer good protection to people against mosquito bites while sleeping. Since Aedes mosquitoes (the primary vector for transmission) are active at dawn and dusk, personal protective measures are recommended particularly at these times of day.
Entomological surveillance should be undertaken to assess the breeding potential of Aedes mosquitoes in containers as well as to monitor insecticide resistance to help select most effective insecticide-based interventions. Insecticide resistance test kits produced by a WHO-coordinated facility in Universiti Sains Malaysia should be procured.
There is no specific treatment for dengue infection, but early detection and access to appropriate healthcare for case management can reduce mortality. Rapid detection of severe dengue cases and timely referrals to tertiary hospitals can reduce mortality. Case surveillance should continue to be enhanced in all affected areas and across the country. Where feasible, resources should be allocated for the strengthening of a sample referral mechanism for the confirmation and sub-typing of dengue virus.
WHO does not recommend that any general travel or trade restrictions be applied to Bangladesh based on the information available for this event.
Further information
- WHO Dengue and severe dengue factsheet. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue
- Hossain, M.S., Noman, A.A., Mamun, S.A.A. et al. Twenty-two years of dengue outbreaks in Bangladesh: epidemiology, clinical spectrum, serotypes, and future disease risks. Trop Med Health 51, 37 (2023). https://doi.org/10.1186/s41182-023-00528-6https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-023-00528-6(link is external)
- DGHS Bangladesh- daily dengue bulletin accessible at https://old.dghs.gov.bd/index.php/bd/home/5200-daily-dengue-status-report
Citable reference: World Health Organization (11 August 2023). Disease Outbreak News; Dengue in Bangladesh. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON481