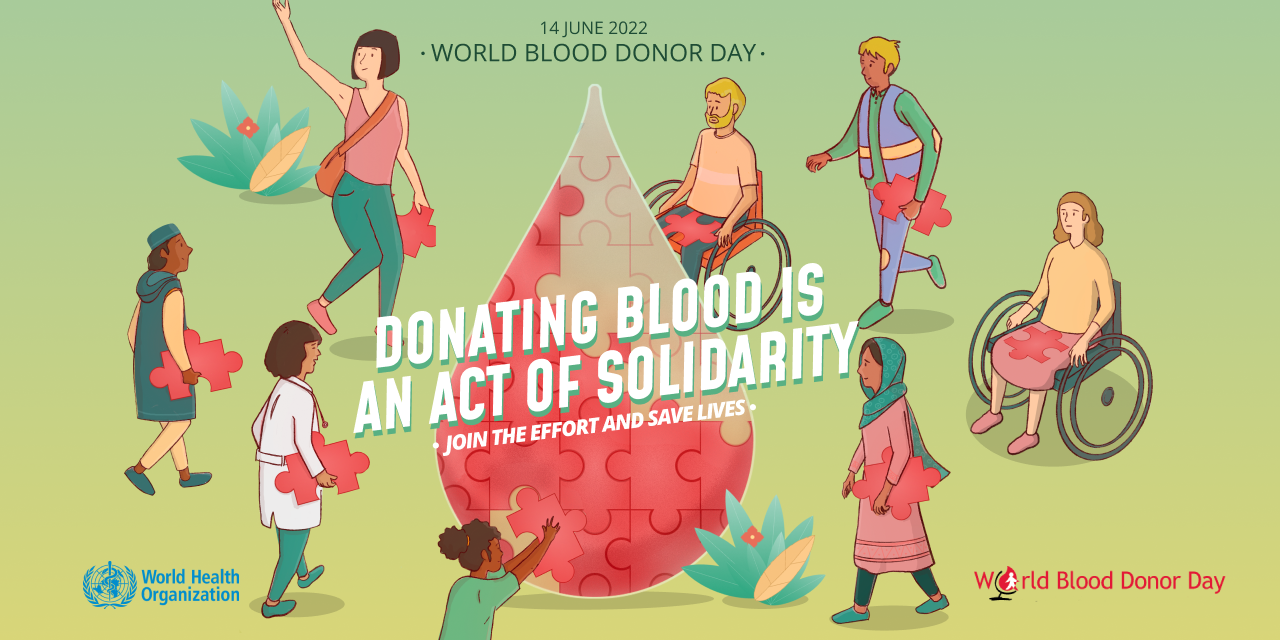
World Blood Donor Day 2022: Donating blood is an act of solidarity. Join the effort and save lives
World Blood Donor Day takes place on 14 June each year. The Day was created to:
- raise global awareness of the need for safe blood and blood products for transfusion;
- highlight the critical contribution voluntary, unpaid blood donors make to national health systems;
- support national blood transfusion services, blood donor organizations and other non-governmental organizations in strengthening and expanding their voluntary blood donor programmes by reinforcing national and local campaigns.
The day also provides an opportunity to call to action governments and national health authorities to provide adequate resources to increase the collection of blood from voluntary, unpaid blood donors and to manage access to blood and the transfusion of those who require it.
Blood and blood products are essential resources for effective management of women suffering from bleeding associated with pregnancy and childbirth; children suffering from severe anaemia due to malaria and malnutrition; patients with blood and bone marrow disorders inherited disorders of haemoglobin and immune deficiency conditions; victims of trauma, emergencies, disasters and accidents; as well as patients undergoing advanced medical and surgical procedures. The need for blood is universal, but access to blood for all those who need it is not. Blood shortages are particularly acute in low- and middle-income countries.
To ensure that everyone who needs transfusion has access to safe blood, all countries need voluntary, unpaid blood donors who give blood regularly. An effective blood donor programme, characterized by wide and active participation of the population, is crucial in meeting the need of blood transfusion during peace time as well as during emergencies or disasters, when there is a surge in demand for blood or when the normal operation of blood services is affected. While an enabling social and cultural atmosphere with strong solidarity facilitates development of an effective blood donor programme, it is also widely acknowledged that the act of blood donation contributes to generating social ties and building a united community.
Focus of this year’s campaign
For 2022, the World Blood Donor Day slogan is “Donating blood is an act of solidarity. Join the effort and save lives” to draw attention to the roles that voluntary blood donations play in saving lives and enhancing solidarity within communities.
The specific objectives of this year’s campaign are to:
- thank blood donors in the world and create wider public awareness of the need for regular, unpaid blood donation;
- highlight the need for committed, year-round blood donation, to maintain adequate supplies and achieve universal and timely access to safe blood transfusion;
- recognize and promote the values of voluntary unpaid blood donation in enhancing community solidarity and social cohesion;
- raise awareness of the need for increased investment from governments to build a sustainable and resilient national blood system and increase collection from voluntary non-remunerated blood donors.
A particular activity that countries in the world are encouraged to implement for this year’s campaign is to disseminate to various media outlets stories of people whose lives have been saved through blood donation as a way of motivating regular blood donors to continue giving blood, and to motivate people in good health who have never given blood to begin doing so.
Other activities that would help promote the slogan of this year’s World Blood Donor Day may include donor appreciation ceremonies, social networking campaigns, special media broadcasts, social media posts featuring individual blood donors with the slogan, meetings and workshops, musical and artistic events to thank blood donors and celebrate solidarity, and colouring iconic monuments red.
Your involvement and support will help to ensure greater impact for World Blood Donor Day 2022, increasing recognition worldwide that giving blood is a life-saving act of solidarity and that services providing safe blood and blood products are an essential element of every health care system. Participation of interested partners is welcome at all levels to make World Blood Donor Day 2022 a global success.
Key facts
- Of the 118.5 million blood donations collected globally, 40% of these are collected in high-income countries, home to 16% of the world’s population.
- In low-income countries, up to 54 % of blood transfusions are given to children under 5 years of age; whereas in high-income countries, the most frequently transfused patient group is over 60 years of age, accounting for up to 76% of all transfusions.
- Based on samples of 1000 people, the blood donation rate is 31.5 donations in high-income countries, 16.4 donations in upper-middle-income countries, 6.6 donations in lower-middle-income countries and 5.0 donations in low-income countries.
- An increase of 10.7 million blood donations from voluntary unpaid donors has been reported from 2008 to 2018. In total, 79 countries collect over 90% of their blood supply from voluntary unpaid blood donors; however, 54 countries collect more than 50% of their blood supply from family/replacement or paid donors.
- Only 56 of 171 reporting countries produce plasma-derived medicinal products (PDMP) through the fractionation of plasma collected in the reporting countries. A total of 91 countries reported that all PDMP are imported, 16 countries reported that no PDMP were used during the reporting period, and 8 countries did not respond to the question.
- The volume of plasma for fractionation per 1000 population varied considerably between the 45 reporting countries, ranging from 0.1 to 52.6 litres, with a median of 5.2 litres.
National blood policy and organization
Blood transfusion saves lives and improves health, but many patients requiring transfusion do not have timely access to safe blood. Providing safe and adequate blood should be an integral part of every country’s national health care policy and infrastructure.
WHO recommends that all activities related to blood collection, testing, processing, storage and distribution be coordinated at the national level through effective organization and integrated blood supply networks. The national blood system should be governed by national blood policy and legislative framework to promote uniform implementation of standards and consistency in the quality and safety of blood and blood products.
In 2018, 73 % of reporting countries, or 125 out of 171, had a national blood policy. Overall, 66% of reporting countries, or 113 out of 171, have specific legislation covering the safety and quality of blood transfusion, including:
- 79% of high-income countries
- 63% of middle-income countries
- 39% of low-income countries.
Blood supply
About 118.54 million blood donations are collected worldwide. 40% of these are collected in high-income countries, home to 16 % of the world’s population.
About 13 300 blood centres in 169 countries report collecting a total of 106 million donations. Collections at blood centres vary according to income group. The median annual donations per blood centre is 1 300 in the low-income countries, 4 400 in lower-middle-income countries and 9 300 in upper-middle-income countries, as compared to 25 700 in high-income countries.
There is a marked difference in the level of access to blood between low- and high-income countries. The whole blood donation rate is an indicator for the general availability of blood in a country. The median blood donation rate in high-income countries is 31.5 donations per 1000 people. This compares with 16.4 donations per 1000 people in upper-middle-income countries, 6.6 donations per 1000 people in lower-middle-income countries, and 5.0 donations per 1000 people in low-income countries.
60 countries report collecting fewer than 10 donations per 1000 people. Of these, 34 countries are in the WHO African Region, four in the WHO Region of the Americas, four in the WHO Eastern Mediterranean region, four in the WHO European Region, five in the WHO South-Eastern Asia Region, and nine in the WHO Western Pacific Region. All are low- or middle-income countries.
Blood donors
Age and gender of blood donors
Data about the gender profile of blood donors show that globally 33% of blood donations are given by women, although this ranges widely. In 15 of the 113 reporting countries, less than 10% of donations are given by female donors.
The age profile of blood donors shows that, proportionally, more young people donate blood in low- and middle-income countries than in high-income countries. Demographic information of blood donors is important for formulating and monitoring recruitment strategies.
Types of blood donors
There are 3 types of blood donors:
- voluntary unpaid
- family/replacement
- paid.
An adequate and reliable supply of safe blood can be assured by a stable base of regular, voluntary, unpaid blood donors. These donors are also the safest group of donors as the prevalence of bloodborne infections is lowest among this group. World Health Assembly resolution WHA63.12 urges all Member States to develop national blood systems based on voluntary unpaid donations and to work towards the goal of self-sufficiency.
Data reported to WHO shows significant increases of voluntary unpaid blood donations in low- and middle-income countries:
- An increase of 10.7 million blood donations from voluntary unpaid donors from 2008 to 2018 has been reported by 119 countries. The highest increase of voluntary unpaid blood donations is in the South-East Asia Region (127%) followed by the Region of the Americas (81%) and Africa (81%). The maximum increase in absolute numbers was reported in the Western Pacific Region (4.15 million donations), followed by South-East Asia (3.05 million) and Africa (1.53 million donations).
- 79 countries collect more than 90% of their blood supply from voluntary unpaid blood donations (38 high-income countries, 33 middle-income countries and eight low-income countries). This includes 64 countries with 100% (or more than 99%) of their blood supply from voluntary unpaid blood donors.
- In 54 countries, more than 50% of the blood supply is still dependent on family/replacement and paid blood donors (eight high-income countries, 36 middle-income countries and 10 low-income countries).
Blood screening
WHO recommends that all blood donations should be screened for infections prior to use. Screening for HIV, hepatitis B, hepatitis C, and syphilis should be mandatory. Blood screening should be performed according to quality system requirements. Of reporting countries, 10 are not able to screen all donated blood for one or more of the above infections.
99.8% of the donations in high-income countries and 99.9% in upper-middle-income countries are screened following basic quality procedures, as compared to 83% in lower-middle-income countries and 76 % in low-income countries. The prevalence of transfusion-transmissible infections in blood donations in high-income countries is considerably lower than in low- and middle-income countries (Table 1).
Table 1. Prevalence of transfusion-transmissible infections in blood donations (Median, Interquartile range (IQR)), by income groups
| HIV | HBV | HCV | Syphilis | ||
| High-income countries | 0.002% | 0.02% | 0.007% | 0.02% | |
| (<0.001% – 0.01%) | (0.005% – 0.12%) | (0.002% – 0.06%) | (0.003% –0.12%) | ||
| Upper middle-income countries | 0.10% | 0.29% | 0.19% | 0.35% | |
| (0.03% – 0.23%) | (0.13% – 0.62%) | (0.07% – 0.36%) | (0.13% –1.10%) | ||
| Lower middle-income countries | 0.19% | 1.70% | 0.38% | 0.69% | |
| (0.04% – 0.62%) | (0.70% – 4.74%) | (0.12% –0.99%) | (0.19% – 1.38%) | ||
| Low-income countries | 0.70% | 2.81% | 1.00% | 0.90% | |
| (0.28% – 1.60%) | (2.00% – 6.02%) | (0.50% – 1.67%) | (0.60% – 1.81%) |
These differences reflect the variation in prevalence among population who are eligible to donate blood, the type of donors (such as voluntary unpaid blood donors from lower risk populations) and the effectiveness of the system of educating and selecting donors.
Blood processing
Blood collected in an anticoagulant can be stored and transfused to a patient in an unmodified state. This is known as ‘whole blood’ transfusion. However, blood can be used more effectively if it is processed into components, such as red cell concentrates, platelet concentrates, plasma and cryoprecipitate. In this way, it can meet the needs of more than one patient.
The capacity to provide patients with the different blood components they require is still limited in low-income countries: 38% of the blood collected in low-income countries is separated into components, 75% in lower-middle-income countries, 96% in upper-middle-income countries, and 96% in high-income countries.
Supply of plasma-derived medicinal products (PDMP)
World Health Assembly resolution WHA63.12 urges Member States to establish, implement and support nationally coordinated, efficiently managed and sustainable blood and plasma programmes, according to the availability of resources, with the aim of achieving self-sufficiency. It is the responsibility of individual governments to ensure sufficient and equitable supply of plasma-derived medicinal products, namely immunoglobulins and coagulation factors, which are needed to prevent and treat a variety of serious conditions that occur worldwide.
Only 56 of 171 reporting countries produce plasma-derived medicinal products (PDMP) through the fractionation of plasma collected in the reporting country. A total of 91 countries reported that all PDMP are imported, 16 countries reported that no PDMP were used during the reporting period, and 8 countries did not respond to the question.
Around 19 million litres of plasma from 45 reporting countries was fractionated for the production of PDMP during the year. This includes around 31% of plasma recovered from the whole blood donations. The volume of plasma for fractionation (and processing for PDMPs) per 1000 population varied considerably between the reporting countries, ranging from 0.1 to 52.6 litres, with a median of 5.2 litres.
Clinical use of blood
Unnecessary transfusions and unsafe transfusion practices expose patients to the risk of serious adverse transfusion reactions and transfusion-transmissible infections. Unnecessary transfusions also reduce the availability of blood products for patients who are in need.
WHO recommends the development of systems, such as hospital transfusion committees and haemovigilance, to monitor and improve the safety of transfusion processes. In this regard:
- 128 countries have national guidelines on the appropriate clinical use of blood: 32 countries in the African region (74% of reporting countries in the region), 23 in the Americas (70%), 12 in the Eastern Mediterranean (67%), 33 in Europe (80%), 9 in the South East Asia (90%), and 19 in the Western Pacific (76%).
- Transfusion committees are present in 48% of the hospitals performing transfusions: 62% in hospitals in high-income countries, 35% in upper-middle-income countries, 31 in lower-middle-income countries and 25% in low-income countries.
- Systems for reporting adverse transfusion events are present in 55% of the hospitals performing transfusions: 74% in hospitals in high-income countries, 35% in upper-middle-income countries, 22% in lower-middle-income countries and 18% in low-income countries,
- 49% of reporting countries have a haemovigilance system. The European region has the highest percentage of countries with haemovigilance systems (81%), followed by the Western Pacific (50%), the Eastern Mediterranean (50%), Africa (40%), South-East Asia (40%), and the Americas (21%).
Blood transfusions
There are great variations between countries in terms of age distribution of transfused patients. For example, in high-income countries, the most frequently transfused patient group is over 60 years of age, which accounts for up to 76% of all transfusions. In low-income countries, up to 54% of transfusions are for children under the age of 5 years.
In high-income countries, transfusion is most commonly used for supportive care in cardiovascular surgery, transplant surgery, massive trauma, and therapy for solid and haematological malignancies. In low- and middle-income countries it is used more often to manage pregnancy-related complications and severe childhood anaemia.
Who can give blood?
Most people can give blood if they are in good health. There are some basic requirements one need to fulfill in order to become a blood donor. Below are some basic eligibility guidelines:
Age
You are aged between 18 and 65.
- In some countries national legislation permits 16–17 year-olds to donate provided that they fulfil the physical and hematological criteria required and that appropriate consent is obtained.
- In some countries, regular donors over the age of 65 may be accepted at the discretion of the responsible physician. The upper age limit in some countries are 60.
Weight
You weigh at least 50 kg.
- In some countries, donors of whole blood donations should weigh at least 45 kg to donate 350 ml ± 10%.
Health
You must be in good health at the time you donate.
You cannot donate if you have a cold, flu, sore throat, cold sore, stomach bug or any other infection.
If you have recently had a tattoo or body piercing you cannot donate for 6 months from the date of the procedure. If the body piercing was performed by a registered health professional and any inflammation has settled completely, you can donate blood after 12 hours.
If you have visited the dentist for a minor procedure you must wait 24 hours before donating; for major work wait a month.
You must not donate blood If you do not meet the minimum haemoglobin level for blood donation:
- A test will be administered at the donation site. In many countries, a haemoglobin level of not less than 12.0 g/dl for females and not less than 13.0 g/dl for males as the threshold.
Travel
Travel to areas where mosquito-borne infections are endemic, e.g. malaria, dengue and Zika virus infections, may result in a temporary deferral.
Many countries also implemented the policy to defer blood donors with a history of travel or residence for defined cumulative exposure periods in specified countries or areas, as a measure to reduce the risk of transmitting variant Creutzfeldt-Jakob Disease (vCJD) by blood transfusion.
Behaviours
You must not give blood:
- If you engaged in “at risk” sexual activity in the past 12 months
- Individuals with behaviours below will be deferred permanently:
- Have ever had a positive test for HIV (AIDS virus)
- Have ever injected recreational drugs.
In the national blood donor selection guidelines, there are more behavior eligibility criteria. Criteria could be different in different countries.
Pregnancy and breastfeeding
Following pregnancy, the deferral period should last as many months as the duration of the pregnancy.
It is not advisable to donate blood while breast-feeding. Following childbirth, the deferral period is at least 9 months (as for pregnancy) and until 3 months after your baby is significantly weaned (i.e. getting most of his/her nutrition from solids or bottle feeding).
More information on eligibility to donate
National eligibility guidelines must be followed when people donate blood in the blood service in specific countries. To find out whether any health conditions, medications, professions or travel history to could affect your ability to give blood, please search for detailed information in the national/local blood services.